Someone with back pain might receive painkillers from his or her primary care physician, then be referred to a physiotherapist, and possibly sent for a scan if the pain continues.
However, has anyone asked where the pain actually started?
“When we take a holistic view, looking at balance, mobility, strength, nutrition, stress, and the person’s overall environment, we’re better able to support recovery,” Dr. Indra Barathan, a functional medicine general practitioner, told The Epoch Times.
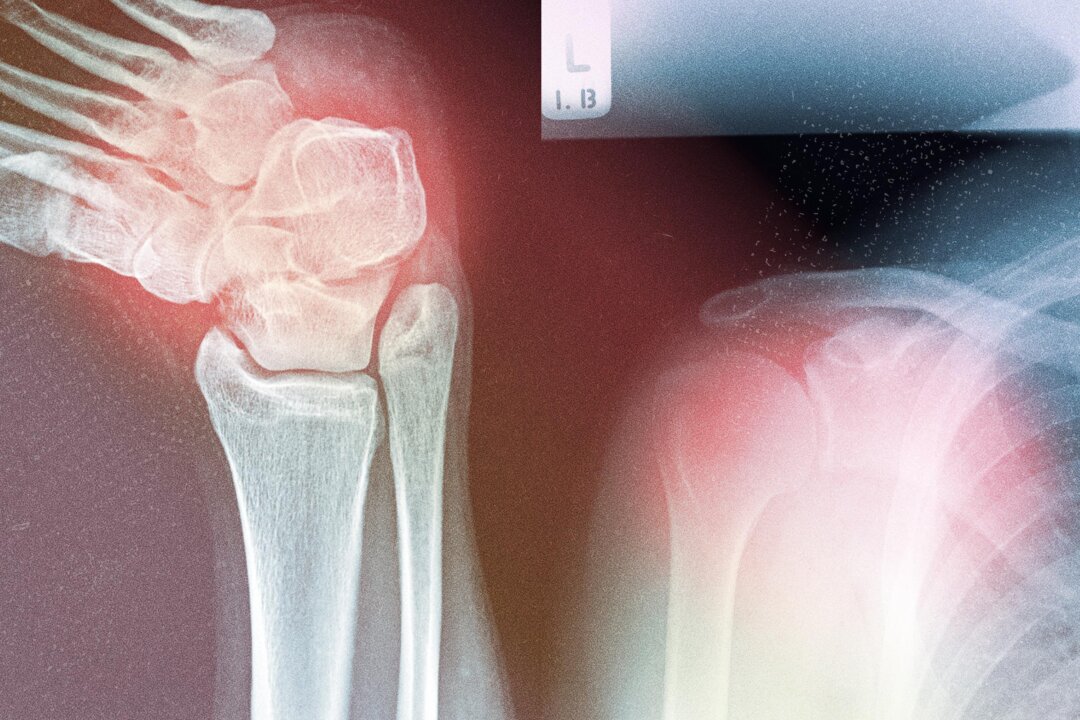
Unfortunately, this isn’t the standard approach for many musculoskeletal conditions such as osteoarthritis, osteoporosis, gout, sarcopenia, and rheumatoid arthritis. These conditions are rising rapidly as the population ages and now affect more than 121 million people in the United States. A shift is needed toward personalized, whole-person support—much of which can be done before serious problems develop.
The Rapid Rise
Chronic musculoskeletal conditions are now the leading cause of disability worldwide. These conditions don’t just affect mobility—they also reduce quality of life and increase the risk of falls, fractures, and hospitalizations.
In 2021, about 607 million people were living with osteoarthritis—a 137 percent increase since 1990. Rheumatoid arthritis and gout have also surged, rising by 125 percent and 150 percent, respectively.
The cost of these conditions is substantial. For example, the average cost of treating a single osteoporotic fracture is more than $21,800.
What’s driving the sharp rise of musculoskeletal conditions?
Aging is a major factor, especially because of the natural loss of muscle and bone strength over time. However, it’s not the only one. Inflammation also plays a central role. Specifically, chronic low-grade inflammation—or “inflammaging”—continues this degenerative cycle, demonstrating how the aging processes converge to promote musculoskeletal decline.
“Inflammation is often at the root of many chronic health problems,” Barathan said.
You can identify it in many conditions that end in “-itis,” such as arthritis and tendinitis, she said.
Inflammation is a normal healing response meant to restore balance. However, when triggers such as poor diet, stress, and environmental factors persist, inflammation can become chronic—leading to ongoing symptoms and multiple diagnoses.
Although workplace injuries, poor posture, and lifting-related strain are common immediate causes of musculoskeletal issues, functional medicine—a health care approach that targets root causes beyond just symptoms—looks deeper.
“Lifestyle factors often predispose people to musculoskeletal problems in the first place,” Barathan said.
For example, poor nutrition and nutrient deficiencies can weaken bones and nerves. A sedentary lifestyle—especially one involving prolonged sitting—can lead to muscle weakness and reduced balance. Chronic stress can further disrupt sleep, nutrition, and movement patterns, affecting concentration, coordination, and resilience, Barathan noted.
“The traditional medical model doesn’t always look at the whole person,” she said.
Barriers to Effective Care
Despite growing awareness and detailed clinical guidelines, delivering consistent, high-quality care remains difficult in real-world settings.
Staff shortages, perceived complexities of treatment, and common misconceptions about treatment further widen the gap between best practice and what patients actually receive.
As Barathan noted, recovery is often more successful when we look beyond the immediate symptoms and consider the root causes. Yet this holistic, person-centered approach is still not standard in most health care settings.
The situation is further complicated by polypharmacy, especially among older adults managing multiple chronic conditions. Interactions between medications—such as between bisphosphonates used for osteoporosis and diuretics or antacids—can undermine treatment. Nonsteroidal anti-inflammatory drugs, commonly used for pain relief, can increase the risk of ulcers and gastrointestinal bleeding.
Medication side effects can also affect the absorption of nutrients such as calcium.
“Corticosteroids, proton pump inhibitors, and diuretics may negatively impact bone health by interfering with how nutrients are absorbed,” Angel Planells, a Seattle-based registered dietitian nutritionist and spokesperson for the Academy of Nutrition and Dietetics, told The Epoch Times.
A Prevention-Focused Approach
Given the limitations of symptom-based care, prevention offers a more sustainable path forward. Many musculoskeletal conditions can be reduced or delayed by addressing the root problems early.
“Lifestyle and nutrition should be considered first-line strategies, for both prevention and treatment,” Planells said.
According to Planells, practical, evidence-based dietary recommendations include:
- Calcium and Vitamin D: Essential for bone strength, with low levels strongly linked to osteoporosis. Aim to get calcium from food sources such as dairy, fortified plant milks, and leafy greens, and vitamin D from sunlight or supplements.
- Protein: Important for preserving muscle mass, especially in older adults, who often don’t eat enough protein, increasing their risk of sarcopenia. Planells recommended eating at least 1 gram of protein per kilogram of body weight each day. Good sources include lean meats, eggs, dairy, legumes, tofu, nuts, and seeds.
- Omega-3 Fatty Acids: Beneficial for joint health due to their anti-inflammatory properties. May be especially helpful in managing rheumatoid arthritis. A Mediterranean-style diet rich in fruits, vegetables, whole grains, fish, nuts, and olive oil is often recommended alongside medical treatment.
- Magnesium, Vitamin K, and Phosphorus: Support bone and muscle function and help maintain structural integrity.
- Low-Sodium and Low-Sugar Soft Drinks: Reducing salt intake and limiting sugary beverages can help prevent calcium loss and support better bone density. Choosing nutrient-dense beverages such as milk and 100 percent juice is encouraged.
“Food first is ideal when possible,” Planells said, referring to getting your nutrients primarily through whole foods rather than pills or powders. This strategy supports better absorption and offers additional benefits such as fiber and protective plant compounds.
However, in cases in which dietary intake isn’t enough—because of medical conditions, age-related changes, or dietary restrictions—supplements may be necessary. Planells advised consulting a health care provider before starting any supplements, noting the potential for drug-nutrient interactions.
Lifestyle changes are equally critical. Regular weight-bearing and resistance exercise helps build bone density, preserve muscle mass, and improve balance. In fact, people who get at least five hours of moderate to vigorous physical activity per week have a lower risk of developing low back, neck, or shoulder pain.
Planells also emphasized quitting smoking and moderating alcohol, as both can weaken bones by interfering with nutrient absorption or bone formation.
Barathan recommended checking key health markers—such as blood glucose, triglycerides, and bone density—to provide a baseline and track progress.
Musculoskeletal decline is not inevitable, Planells said.
“Many age-related changes can be slowed or even reversed with the right interventions,” he said.