Lower back pain refers to pain or discomfort between the lower margin of the ribs and the top of the buttocks.
It affects most American adults at some point and is the most common musculoskeletal condition worldwide—and the leading cause of disability globally.
In most cases, lower back pain improves on its own with rest, gentle movement, and self-care, though it can sometimes be quite severe and limiting. Fortunately, many natural approaches can help relieve symptoms and support recovery, and the symptoms can often be prevented through healthy habits and lifestyle choices.
[epoch_component type=”photo_gallery” position=”center” section_title=”(Illustration by The Epoch Times, Shutterstock)” width=”900″ items=”5951273,” image_stays=”false” stays_for_paragraphs=””][/epoch_component]
[shortcut_anchor id=”anchor_1764377398648″ label=”Symptoms”]What Are the Specific Symptoms of Lower Back Pain?[/shortcut_anchor]
Lower back pain can range from a dull ache to sharp, tearing, or burning pain.
Common symptoms that appear with—or even before—lower back pain begins include:
- Morning Stiffness: Stiffness in the lower back upon waking
- End-of-Day or Post-Exercise Stiffness: The lower back feels tight or sore after a day of activity
- Discomfort When Rising or Standing: Pain or stiffness when standing up from sitting or while standing
- Muscle Tightness: Tightness in the hamstrings or calves, even without recent exercise
Acute lower back pain is short-term, lasting from a few days to a few weeks. It accounts for most cases of lower back pain and often resolves on its own with self-care. Chronic lower back pain persists for 12 weeks or longer, even after the initial cause has been treated. About 20 percent of people with acute lower back pain develop chronic pain within a year. Persistent pain does not always indicate a serious underlying condition, and sometimes no clear cause can be identified.
When to Talk to Your Doctor
You may want to talk with your doctor if you experience persistent, severe, or worsening pain, have tingling or numbness, or other concerning symptoms like sudden weight loss. You may also want to see your doctor if you have a history of cancer, are prone to infections, or use certain medications such as intravenous drugs.
If any of the following symptoms occur, seek immediate medical attention:
- Sharp Pain: A sharp pain may signal a torn muscle or ligament, or a problem with an internal organ in the back or side
- Radiating Pain: Radiating pain can indicate nerve compression
- Sudden Leg Weakness: Many conditions may cause sudden weakness in the legs, including a stroke
- Incontinence: Loss of bowel or bladder control along with back pain may indicate serious nerve compression or spinal infection, such as discitis or meningitis
- Numbness or Tingling in the Groin or Glutes: Known as saddle anesthesia, this symptom can signal a serious nerve or spinal condition
- Trauma: A recent injury, such as a fall, especially if there are bruising or cuts, or scrapes associated with the pain
[shortcut_anchor id=”anchor_1764377417594″ label=”Causes”]What Causes Lower Back Pain?[/shortcut_anchor]
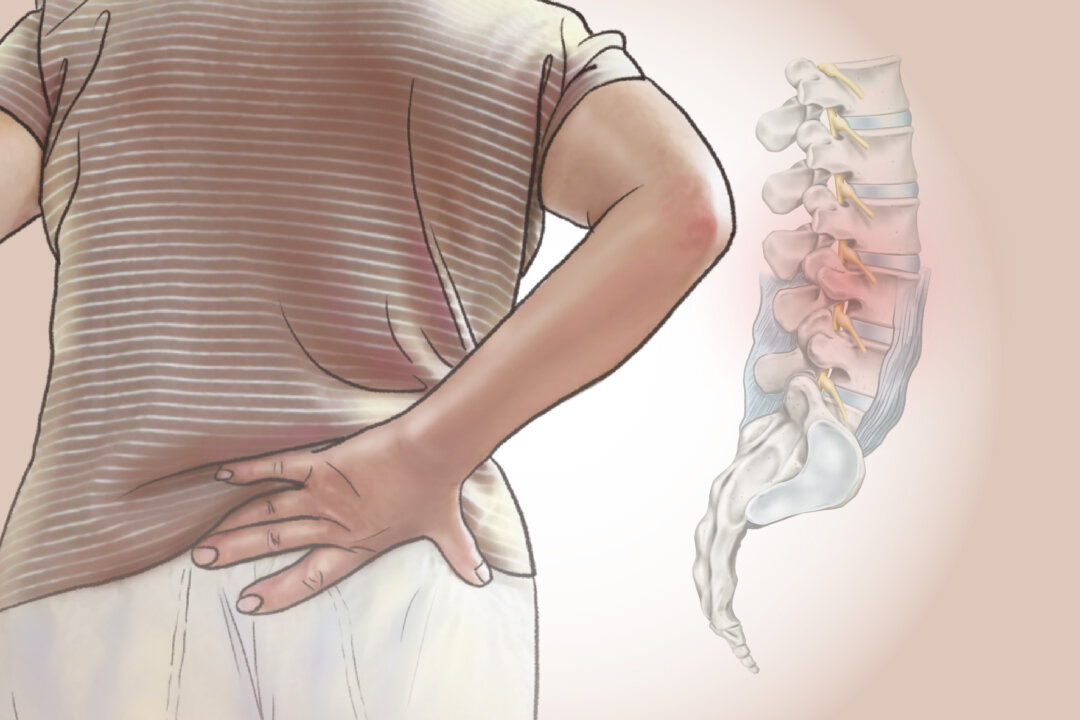
The lumbar spine in the lower back consists of five vertebrae situated between the ribs and pelvis. Intervertebral discs cushion these bones and act as shock absorbers. Each disc has a tough outer layer, called the annulus, surrounding a jelly-like center called the nucleus, held in place by strong ligaments. Five lumbar and five sacral pairs of spinal nerves originate in the lower back, connecting the spine to the rest of the body.
Lower back pain can be categorized into two main types: specific and nonspecific back pain.
1. Specific Causes and Risk Factors
For specific lower back pain, there are many different causes, including:
Muscle Pain
A common cause of lower back pain is muscle soreness from physical activity, which can occur when muscles, tendons, or ligaments become overstretched or injured.
Disc Injuries
When lower back pain is persistent, severe, or accompanied by other symptoms, it may indicate a problem with intervertebral discs.
Discs wear down and shrink with age, and facet joints—small joints connecting the vertebrae—may rub together, leading to pain and stiffness. Aging can also cause small tears in the outer layer of the disc.
Disc Herniation: A herniated, or “slipped” disc happens when the soft inner material pushes through a weakened outer layer and can sometimes press on spinal nerves. Herniated discs commonly occur after lifting, pulling, bending, or twisting.
Bone and Facet Joint Problems
Pain can result from injuries to the bones of the spine, including fractures caused by a fall, accident, or osteoporosis.
Wear and tear on the facet joints, known as osteoarthritis, can also contribute to back problems.
Nerve Problems
Two common issues include:
Spinal stenosis, the narrowing of the spinal canal, can compress the spinal cord and nerves.
Scoliosis, an abnormal spinal curve, can also put pressure on nerves and lead to pain.
Other Medical Conditions
Kidney stones, fibromyalgia, endometriosis, piriformis syndrome, spinal tumors or metastases from cancers such as blood, breast, gastrointestinal, kidney, lung, ovarian, or prostate cancer, and osteoporosis can cause lower back pain.
Congenital Issues
Conditions such as skeletal irregularities and spina bifida can cause lower back pain.
Other Problems
Sometimes lower back pain stems from everyday factors you might not immediately suspect, including posture habits, pregnancy, or even changes in the weather.
- Poor Posture: Poor posture places extra mechanical stress on the lower back.
- Weather Changes: Shifts in barometric pressure and outdoor temperature can affect the spine and joints, making them stiffer and more prone to pain.
- Pregnancy: Pregnancy can cause lower back pain because of added weight, posture changes, and hormonal loosening of ligaments in the spine and pelvis.
2. Nonspecific Causes and Risk Factors
Nonspecific lower back pain, which has no identifiable cause, accounts for about 90 percent of cases. Several factors can increase the risk of developing nonspecific lower back pain, including the following:
Lifestyle Factors
Your daily routines—how you sit, move, work, and manage stress—can play a major role in triggering or worsening lower back pain.
- Stress and Depression: Stress and depression can intensify the perception of pain, while chronic lower back pain can contribute to these psychological issues.
- Obesity: Extra body weight adds stress to the spine, accelerating wear and tear.
- Sitting Uncomfortably: Sitting in an uncomfortable chair for extended periods, or driving long distances without breaks, can contribute to back pain.
- Occupation: Jobs that require heavy lifting, bending, twisting, or exposure to whole-body vibration, such as truck driving or operating a sandblaster, can increase risk.
- Cycling: Younger riders, cyclists with higher body mass, and those who practice mountain biking report lower back pain more often.
- Smoking: Smoking increases inflammation and slows healing, contributing to lower back pain.
Other Risk Factors
The majority of lower back pain develops after age 30. The highest number of cases occurs between ages 50 and 55. Episodes of recurrent lower back pain become more common with age, and women tend to experience lower back pain more frequently than men.
[shortcut_anchor id=”anchor_1764377491476″ label=”Diagnosis”]How Is Lower Back Pain Diagnosed?[/shortcut_anchor]
During the medical history, a health care provider asks about details of the pain and looks for significant signs on the physical exam. Diagnostic tests are generally not needed initially unless specific symptoms are present.
Diagnostic Tests
When symptoms persist or raise red flags, your health care provider may recommend diagnostic tests to better understand the source of your lower back pain.
- Bone Scans: Bone scans detect fractures, infections, or bone disorders by highlighting abnormal bone activity.
- Imaging Tests: Imaging is warranted when there are red flag symptoms such as potential fractures or cancer, persistent symptoms, or signs pointing to a specific structural problem. X-rays show arthritis and fractures, while MRI and CT scans reveal issues involving discs, bones, and soft tissues such as muscles, tendons, ligaments, nerves, and blood vessels.
- Discography: Discography involves injecting dye into a suspected spinal disc to reproduce pain and visualize damage on CT scans.
- Electrodiagnostic Tests: Electrodiagnostic tests help detect nerve problems affecting the back and legs.
- Myelograms: Myelograms use a contrast dye injected into the spinal canal to improve X-ray or CT imaging and help detect spinal cord or nerve compression from herniated discs or fractures.
- Blood Tests: Blood tests measure blood cell levels and inflammation markers. They are not routinely used for back pain but may help check for inflammation, infection, cancer, or arthritis.
[shortcut_anchor id=”anchor_1764377509132″ label=”Treatments”]What Are the Treatments for Lower Back Pain?[/shortcut_anchor]
For lower back pain, doctors usually aim to identify the cause and determine whether symptoms can be improved with simple measures such as ice, mild painkillers, physical therapy, and exercise. Most people recover within four to six weeks.
Treatments for lower back pain aim to relieve discomfort, restore function, and address underlying causes through a combination of self-care, therapy, and medical interventions.
1. Medications
Several types of medicines are used to treat lower back pain, including:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs such as aspirin, ibuprofen, and naproxen reduce pain and inflammation.
- Steroids: Steroids can be taken orally or injected into the spine to provide a strong anti-inflammatory effect.
- Muscle Relaxers: Muscle relaxers can ease muscle tension and pain, but may cause drowsiness, so avoid driving or tasks requiring alertness while taking them.
2. Rehabilitation
If your pain persists for more than a month, your doctor may refer you to a physiatrist, physical therapist, occupational therapist, or a bone and spine specialist, such as an orthopedist or neurosurgeon. Treatment is often tailored to how long symptoms have been present, with approaches generally falling into three stages based on lower back pain duration.
- Acute Stage: Focuses on patient education, reassurance, maintaining normal activity as much as possible, avoiding bed rest, and using NSAIDs when appropriate.
- Subacute Stage: Introduces structured exercise and may include cognitive behavioral therapy to address fear-avoidant behaviors and support recovery.
- Chronic Stage: Uses more specific exercise programs and specialized treatments tailored to the individual patient’s needs to improve long-term function and reduce pain.
3. Cognitive Behavioral Therapy (CBT)
CBT can be an effective approach for managing chronic lower back pain by addressing the psychological and behavioral factors that influence pain perception. CBT helps people recognize and change negative thought patterns, reduce fear-avoidant behaviors, and develop healthier coping strategies for dealing with pain. A 2022 meta-analysis showed that CBT improves confidence in managing pain and reduces fear-avoidance and disability. Often, CBT is used alongside other treatments.
4. Injections
For certain types of back pain, targeted injections can provide temporary relief by calming inflamed or irritated tissues.
- Trigger Point Injections: Local anesthetic, often combined with a corticosteroid, is injected into tight, knotted muscles.
- Epidural Steroid Injections: Steroids are injected into the lumbar epidural space to temporarily reduce inflammation.
- Radiofrequency Ablation: A heated electrode destroys pain-carrying nerve fibers.
5. Implanted Nerve Stimulators
For chronic or hard-to-treat back pain, implanted nerve stimulators offer another option by interrupting pain signals before they reach the brain.
- Spinal Cord Stimulation: An implanted device sends low-voltage electrical impulses that block pain signals.
- Dorsal Root Ganglion Stimulation: Targeted signals are delivered to nerve clusters that carry pain signals.
- Peripheral Nerve Stimulation: Electrical pulses are delivered to specific nerves to create tingling sensations that help relieve pain.
6. Transcutaneous Electrical Nerve Stimulation (TENS)
TENS uses a small battery-powered device with electrodes placed on the skin over the painful area. These electrodes deliver electrical impulses that help block or alter the perception of pain.
7. Traction
Traction uses weights and pulleys to apply a steady or intermittent force to gently realign the spine. It may provide temporary pain relief, but symptoms often return once the traction is stopped.
8. Chiropractic Care
In the United States, chiropractors are well qualified to diagnose, treat, and help manage care for people with lower back pain. People with chronic back and neck pain often report positive experiences with chiropractic care. In an earlier study, more frequent chiropractic visits led to greater short-term improvement in chronic lower back pain. After four weeks, people who received more sessions, about three to four times per week, had noticeably larger reductions in pain and disability. By 12 weeks, differences between groups were less clear.
9. Spinal Manipulation
Spinal manipulation is a hands-on or device-assisted technique that applies a controlled thrust to a spinal joint, moving it beyond its normal range, unlike spinal mobilization, which does not use a thrust. In a 2017 meta-analysis of 15 studies involving nearly 1,700 participants with acute lower back pain, spinal manipulative therapy provided modest short-term improvements in pain and function, with only temporary minor muscle or joint discomfort.
10. Physical Therapy
Your doctor may refer you to a physical therapist or occupational therapist, who first focuses on pain relief and then teaches ways to prevent future back pain.
11. Surgery
Except for emergencies or other serious conditions, surgery is considered only after six to 12 months of unsuccessful nonsurgical treatments, when the source of pain is clearly identified, and surgery is likely to help.
The surgical options are:
- Spinal Fusion: A spinal fusion fuses painful vertebrae into a single bone to stop motion and reduce pain. It is used for spinal instability, scoliosis, or severe disc degeneration. Bone grafts, screws, rods, or cages stabilize the spine while it heals.
- Disc Replacement: A disc replacement replaces a damaged disc with an artificial one to maintain flexibility and motion, usually in the lower spine. Effectiveness compared with fusion is still debated.
- Discectomy: A discectomy removes the damaged portion of a herniated disc to relieve nerve pressure and sciatic pain.
- Laminectomy: A laminectomy removes thickened ligaments and bone spurs compressing nerves to reduce spinal canal pressure and nerve pain.
- Kyphoplasty or Vertebroplasty: These procedures inject cement into fractured vertebrae to stabilize osteoporotic compression fractures and reduce sharp pain.
- Foraminotomy: A foraminotomy enlarges the opening where a nerve root exits the spinal canal. Through a small incision, the surgeon removes small portions of bone or tissue causing the blockage, relieving pressure on the affected nerve.
12. Herbs
Consult an appropriate professional, such as a traditional Chinese medicine (TCM) practitioner or herbalist, before trying any medicinal herbs.
- Bu Shen Tong Luo: Bu Shen Tong Luo, consisting of white peony root, cyathula root, salvia root, earthworm, and other herbal ingredients, has been traditionally used in China to treat lower back pain. A 2024 study involving 71 patients with lower back pain found this herbal formula to be as effective as a type of NSAID in treating symptoms.
- Willow Bark: Willow bark extract was studied in 191 people with flare-ups of chronic lower back pain; after four weeks, 39 percent of participants taking a higher dose of willow bark extract were pain-free, with some feeling relief within the first week.
13. Acupuncture
Acupuncture has been shown to effectively reduce lower back pain, with many people using it for chronic lower back pain. Clinical guidelines from the American College of Physicians recommend acupuncture as an initial treatment option for both chronic and acute lower back pain. A study published in September involving 800 older adults with chronic lower back pain found that acupuncture significantly improved pain and disability over six and 12 months compared with usual medical care alone.
14. Moxibustion
Moxibustion is a traditional Chinese therapy that involves burning dried mugwort near or on specific acupuncture points. Research shows that both single and combined moxibustion treatments can decrease levels of key inflammatory chemicals to achieve pain relief. With rare and short-lived side effects, moxibustion is considered a relatively safe treatment option.
- Ma’s Bamboo-Based Moxibustion: Bamboo tubing and herbal compounds are used to apply heat and medicinal ingredients to acupoints. A 2024 study found Ma’s moxibustion to be as effective as acupuncture for lumbar disc herniation.
- Huolong (“Fire Dragon”) Moxibustion: Traditional moxibustion is combined with herbal steaming. A 2019 study showed reduced pain and improved back function after three weeks.
[shortcut_anchor id=”anchor_1764377554028″ label=”Lifestyle Approaches”]What Are the Natural and Lifestyle Approaches to Lower Back Pain?[/shortcut_anchor]
Some of the following approaches are recommended as first-line interventions for lower back pain.
1. Self-Care Tips
Current U.S. and international guidelines note that most people with lower back pain experience significant improvement within the first month regardless of the specific exercises or techniques they use.
These guidelines recommend avoiding bed rest and encourage resuming normal activities—including work, lifting, and bending—as tolerated.
Temporary restrictions, such as limiting heavy lifting or prolonged bending, are now reserved for more severe cases and tailored to the individual patient.
These recommendations are aligned with clinical guidance from sources such as the American College of Occupational and Environmental Medicine.
To help reduce stress-related back pain, relax both your mind and muscles. Practice deep breathing for 10 to 15 minutes, focus on enjoyable activities or hobbies, spend time with friends, read, or listen to music.
2. Exercises
Contrary to common belief, extended bed rest is not recommended for lower back pain. If there are no serious warning signs, performing exercises helps maintain back and abdominal muscle strength and supports recovery.
- Light Aerobic Activity: Activities such as walking, swimming, or using a stationary bike improve blood flow, promote healing, and strengthen back and abdominal muscles.
- Walking: In a study published in June involving over 11,000 people, walking reduced the risk of chronic lower back pain. Walking 78 to 100 minutes per day lowered the risk by 13 percent, and 125 minutes or more lowered it by 23 percent compared with walking less than 78 minutes.
- Stretching and Strengthening Exercises: Movements such as the knee-to-chest stretch and the cat-cow stretch help support the back.
- Pilates: A 2024 meta-analysis of 19 studies found that Pilates can reduce lower back pain more effectively than performing no exercise or general, nonspecific exercises. It improves core muscle strength and activation. A 2022 meta-analysis recommended including Pilates in exercise programs for people with lower back pain to achieve the greatest overall benefit.
3. Tibetan CheeZheng Pain-Relieving Plaster
A 2021 meta-analysis involving nine studies with nearly 1,700 patients found that this over-the-counter herbal patch could reduce pain and improve movement in acute lower back pain. When combined with the pain medication diclofenac, the patch provided greater pain relief than diclofenac alone. It also helped more people become pain-free compared with standard NSAID medications.
4. Meditation
Meditation has been shown to significantly reduce pain. A 2022 meta-analysis of 12 studies with more than 1,100 participants found that safe meditation-based therapies can help manage chronic lower back pain by reducing pain and discomfort. Studies also show that mindful meditation can reduce pain severity in people with nonspecific chronic lower back pain, including severe pain, and can enhance pain tolerance.
5. Aromatherapy
A 2023 study showed that aromatherapy massage using frankincense and myrrh essential oils can be added alongside medical treatment to help reduce pain and improve daily functioning in people with chronic lower back pain. Essential oil therapy can also help reduce stiffness. In another 2023 study, inhaling rose geranium essential oil reduced pain, anxiety, and stress in people with lumbar spinal stenosis experiencing moderate to severe pain.
6. Yoga
For lower back pain, yoga is particularly beneficial for strengthening the muscles that support the spine. A 2022 meta-analysis found that yoga can reduce lower back pain, with most benefits lasting long-term. In terms of lower back pain treatment, yoga is as effective as other active treatments such as exercise. People with poorer physical health at baseline tend to experience greater improvements in lower back pain and function from practicing yoga.
7. Dancing
A 2022 study found that ballet and hip-hop dancers showed significant improvements in lower back pain intensity, habitual posture, core muscle strength, and lumbar motor control, with pain decreasing and posture and core strength improving noticeably.
Another study published in June involving 40 women found that dance therapy was more effective than conventional treatment for chronic lower back pain, improving functionality, balance, body awareness, and reducing pain and fall risk.
[shortcut_anchor id=”anchor_1764377567788″ label=”Mindset”]How Does Mindset Affect Lower Back Pain?[/shortcut_anchor]
Mindset and emotional state play a major role in lower back pain, as chronic stress, anxiety, or repressed emotions can keep the brain in a high-alert “fight-or-flight” mode, causing stress hormones to trigger pain signals even without a physical threat.
Over time, these signals can become ingrained in the nervous system, leading to chronic back pain that reflects emotional rather than structural issues. This highlights the mind-body connection and the importance of consciously addressing emotional stress.
[shortcut_anchor id=”anchor_1764377577900″ label=”Prevention”]How Can I Prevent Lower Back Pain?[/shortcut_anchor]
You can use the following tips to prevent lower back pain:
Daily Habits and Posture
Small adjustments to how you sit, stand, and move throughout the day can make a significant difference in preventing or easing lower back pain.
- Maintain good posture by sitting up straight, keeping both feet on the floor, and avoiding slouching.
- Avoid sitting or standing in one position for too long; alternate positions regularly.
- Use an ergonomic chair with an adjustable seat, back, and armrests, and place a small pillow or rolled towel behind your lower back.
- Place a stool under your feet while sitting so your knees are higher than your hips.
- Avoid high heels and choose cushioned footwear.
- When driving long distances, take breaks every hour to walk and stretch.
- Sleep on your side with your knees pulled up in a fetal position to help open the spinal joints and reduce pressure by lessening spinal curvature. Use a firm mattress or surface for better support.
Lifting and Bending
Using proper lifting and bending techniques helps protect your spine and reduces the risk of straining your lower back.
- Avoid lifting heavy or awkward objects.
- Stand close to the object and spread your feet for a stable base.
- Bend at your knees, not at your waist, and tighten your abdominal muscles.
- Hold objects close to your body and lift with your legs, not your back.
- Avoid twisting while lifting, lowering, or carrying objects.
Exercise and Core Strength
Strengthening key muscle groups and staying active supports your spine, improves stability, and lowers your risk of recurring back pain.
- Strengthen abdominal, glute, hip, and lower back muscles to support the spine.
- Engage in regular physical activity to maintain a healthy weight and help avoid falls.
- Quit or avoid smoking to help reduce spinal degeneration risk.
- Learn relaxation techniques.
- Walk frequently to promote spinal mobility and circulation.
[shortcut_anchor id=”anchor_1764377591149″ label=”Complications”]What Are the Possible Complications of Lower Back Pain?[/shortcut_anchor]
If left untreated, lower back pain can progressively worsen. Possible complications include the following:
- Diabetes and Heart Disease: People with lower back pain may reduce their physical activity, which can raise the risk of diabetes and heart disease.
- Radiculopathy: Narrowing of the openings where nerve roots exit is a common cause of radiculopathy. This narrowing is often due to stenosis, bone spurs, disc herniation, or similar degenerative changes.
- Cauda Equina Syndrome: A rare but serious condition where nerve compression at the base of the spinal cord causes bowel or bladder dysfunction, saddle anesthesia, and potentially permanent nerve damage if untreated.
- Psychological Issues: Persistent pain can lead to mental health challenges such as anxiety and depression.