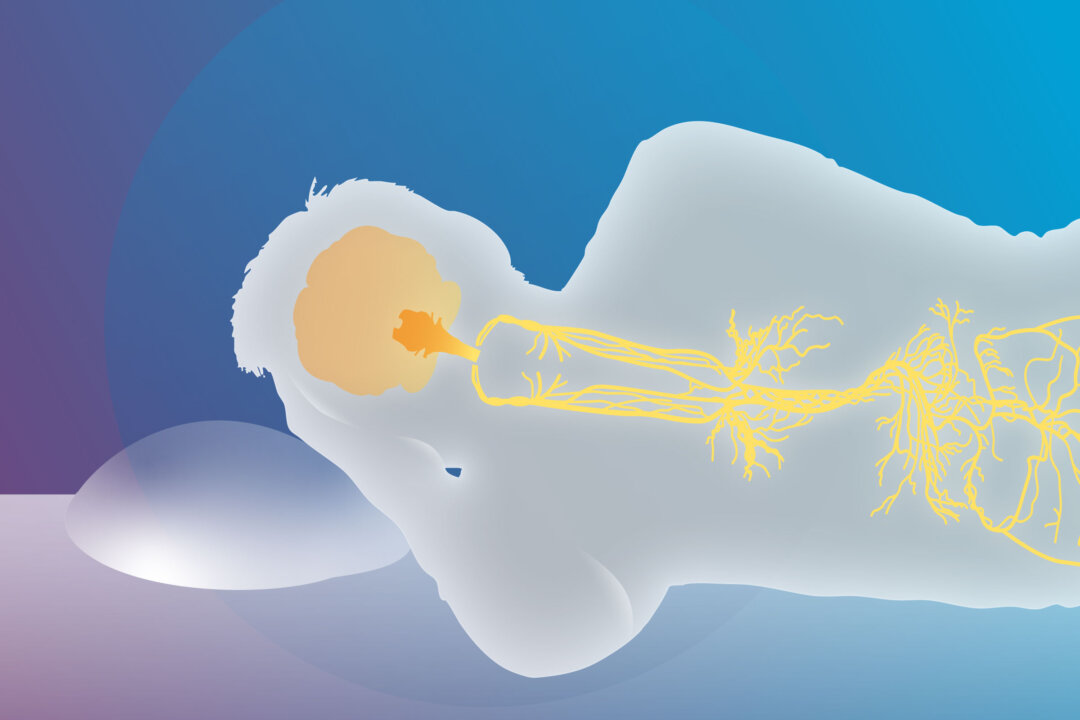
Stimulating the vagus nerve may help people with insomnia sleep better by calming the nervous system and encouraging natural sleep rhythms. Vagus nerve stimulation (VNS)—either mechanically with devices or by breathwork—is increasingly being explored as an alternative to conventional sleep treatments.
In an interview with The Epoch Times, Dr. Priyal Modi, an integrative medical doctor and advanced breathwork practitioner, recalled a patient who was always in a state of fight-or-flight response.
“He was always on guard, his body was rigid, and he had difficulty falling and staying asleep.”
To help, she designed a wind-down routine that created a sense of calm and safety in the man’s surroundings and within his body, using vagus nerve stimulation.
“Over time, his body began to ease and soften, and he cultivated a sense of safety within himself that was reflected in his sleep patterns.”
How VNS Affects Sleep
“Insomnia often stems from the body being stuck in a state of hyperarousal, when the nervous system continues running in fight-or-flight mode and can’t shift into the calm, safe state needed for sleep,” Modi said.
By stimulating the vagus nerve, the parasympathetic state of rest and digest is activated and sympathetic overactivity is reduced, influencing key brain areas involved in sleep–wake cycles and stress responses.
VNS can also alter levels of GABA and serotonin, neurotransmitters critical for sleep regulation, and can further boost deep sleep brain waves.
Mechanical Stimulation
A meta-analysis published in May in Neuromodulation found that transcutaneous auricular vagus nerve stimulation (taVNS) significantly relieved insomnia. By examining results from six clinical trials involving more than 300 patients, researchers found that taVNS improved sleep quality, made it easier to fall asleep, and helped people stay asleep longer.
TaVNS mechanically stimulates the vagus nerve through the skin of the outer ear using a small device that delivers gentle electrical pulses. Unlike implanted devices, which have been linked to side effects such as sleep apnea and heart complications, taVNS is non-invasive, cost-effective, and portable.
The benefits of taVNS extend beyond short-term sleep gains. A Chinese trial published in JAMA Network Open, involving 72 participants, showed that eight weeks of twice-daily taVNS improved sleep quality in patients with chronic insomnia disorder and sustained those improvements for 12 weeks after treatment ended. These lasting effects may be due to the ability of taVNS to reduce anxiety, depression, and fatigue, which are common contributors to insomnia.
People using taVNS should first confirm the condition of chronic insomnia and rule out other sleep disorders, such as sleep apnea, Dr. Yu Wang, a physician researcher who studies insomnia and VNS, told The Epoch Times.
He recommended using a certified taVNS device. Begin with low intensity and gradually increase to a comfortable, tolerable level.
“Stimulate the cymba conchae—the ear region rich in vagus nerve fibers—for 30 minutes, twice daily, at least five days per week,” Wang said.
Consistency is key as clinical trials show meaningful improvements after four to eight weeks of regular use, he added.
Vagus nerve stimulation isn’t limited to devices—breathing practices can have similar effects.
Breathwork
When good sleepers transition from wakefulness to sleep, their breathing naturally slows and becomes more regular. By intentionally shifting our breath in the same way, we can encourage sleep to come more easily.
Diaphragmatic breathing, for example, slows the breath, lowers stress hormones, and calms the nervous system. Also known as “belly breathing,” this practice involves the active use of your diaphragm—the large muscle located under your lungs—to draw air deeply into your lungs. As you inhale, your belly rises instead of your chest, allowing more oxygen in and triggering the body’s relaxation response.
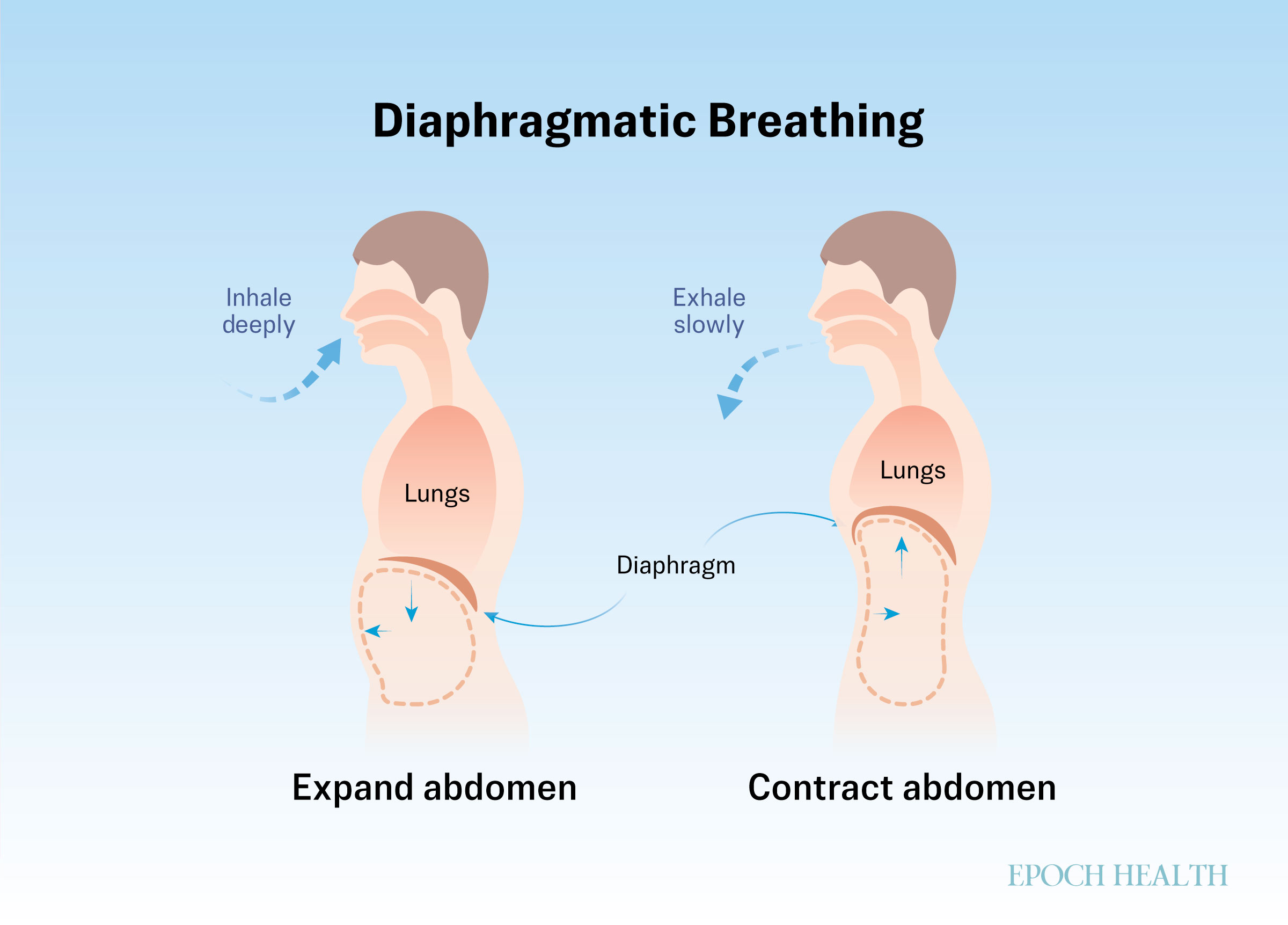
Diaphragmatic breathing boosts parasympathetic activity throughout the night, supporting sleep quality. A study published in Sleep Medicine found that four weeks of diaphragmatic breathing resulted in improved sleep quality, increased sleep duration, fewer sleep disturbances, and reduced daytime dysfunction.
In the study, breathing sessions were sequenced as follows:
- First 5 Minutes: Sit with your shoulders relaxed, legs open, and arms resting naturally at your sides. Close your eyes and focus on your present feelings.
- Next 20 Minutes: Abdominal breathing. Inhale deeply through the nose, contract the diaphragm, relax the abdominal muscles, and expand the abdomen. Exhale slowly through your mouth, relax your diaphragm, and contract your abdominal muscles, and pull your abdomen in.
- Final 5 Minutes: Close your eyes, focus on your present feelings, and relax the entire body.
Participants were encouraged to practice at least once per day.
Our body and nervous system respond well to routine and consistency. It’s more beneficial to have daily practices of five to 10 minutes rather than longer practices inconsistently, Modi noted.
She suggested first, to begin with with breath awareness—simply observing the rhythm and flow of your breath without trying to change it. This method brings you into the present moment, promoting a sense of calm and safety.
Second—to stimulate the vagus nerve—she suggested exhaling twice as long as you inhale. Alternatively, you can breathe in through your nose and then out through your nose or pursed lips.
Just a few minutes of breathing can downregulate the nervous system, Modi said.
“Once you start to understand the science and the nervous system, you can start to piece things together and have a bigger appreciation of the impact of breathwork,” functional breath coach Ross Austen told The Epoch Times.
Austen recommended three other breathwork practices that can improve sleep:
- Cadence Breathing: Inhale for three seconds, hold for three seconds, exhale for six seconds, hold for three seconds, and repeat.
- 478 Breathing: Inhale for four seconds, hold for seven seconds, exhale for eight seconds, and repeat.
- Physiological Sigh: Deeply inhale, immediately followed by a second inhale, then sigh the breath out.
Integrate With Other Sleep Strategies
Both mechanical VNS stimulation and stimulation via breathwork need to be integrated into an overall approach to health, according to the experts.
“TaVNS is not a standalone cure and works best as part of a comprehensive sleep management plan, including cognitive-behavioral therapy for insomnia and lifestyle modifications,” Wang said.
“Always listen to your body to understand which practices work best for your nervous system and how you respond to each technique,” Modi said.
For someone using breathwork to improve sleep, a structured routine can help.
She shared the following example of a well-rounded structure to improve sleep:
- Go to bed and wake up at the same time every day (when possible).
- Avoid meals within three hours of bedtime.
- Wind down one hour before sleep—screens off.
- Do gentle stretches and slow breathing.
- Journal or write down what you’re grateful for.
- Perform five to 10 minutes of extended exhale breathing, humming, or yoga nidra (a guided meditation).
- Take magnesium supplementation in the evening to support muscle relaxation and calm the nervous system.
- Get direct sunlight within 30 to 60 minutes of waking to help reset the circadian rhythm and regulate melatonin release, making it easier to fall asleep at night.
Even those who sleep through the night but still wake up tired may benefit, as the sleep may not be fully restorative.
How quickly someone notices improvements varies depending on the state of their nervous system, lifestyle, and general health. Some people may notice shifts within days, while others may need weeks of regular practice, Modi said.
“The key is patience and consistency, like training any muscle, your vagus nerve needs gentle, regular engagement to bring lasting sleep improvements.”