Forgetfulness in midlife is often chalked up to stress or age. However, research shows that blood pressure may be one of the clearest predictors of how well the brain is holding up.
In the first major update of the U.S. hypertension guidelines since 2017, the American Heart Association and American College of Cardiology urge doctors to act sooner, treating even modest elevations as threats to both heart and brain health.
The goal is to give doctors and patients earlier, more-tailored strategies to help ease the toll of heart disease, kidney disease, diabetes, and dementia, Dr. Daniel W. Jones, chair of the guideline committee, said in a statement.
“High blood pressure is the most modifiable risk factor for stroke and brain complications,” Dr. Shyam Prabhakaran, neurology chair at the University of Chicago, told The Epoch Times. “It affects the brain in silent ways. The brain doesn’t regenerate, so over decades, those injuries take a toll. That’s why putting brain health at the forefront of these guidelines is so important.”
The Silent Threat to the Brain
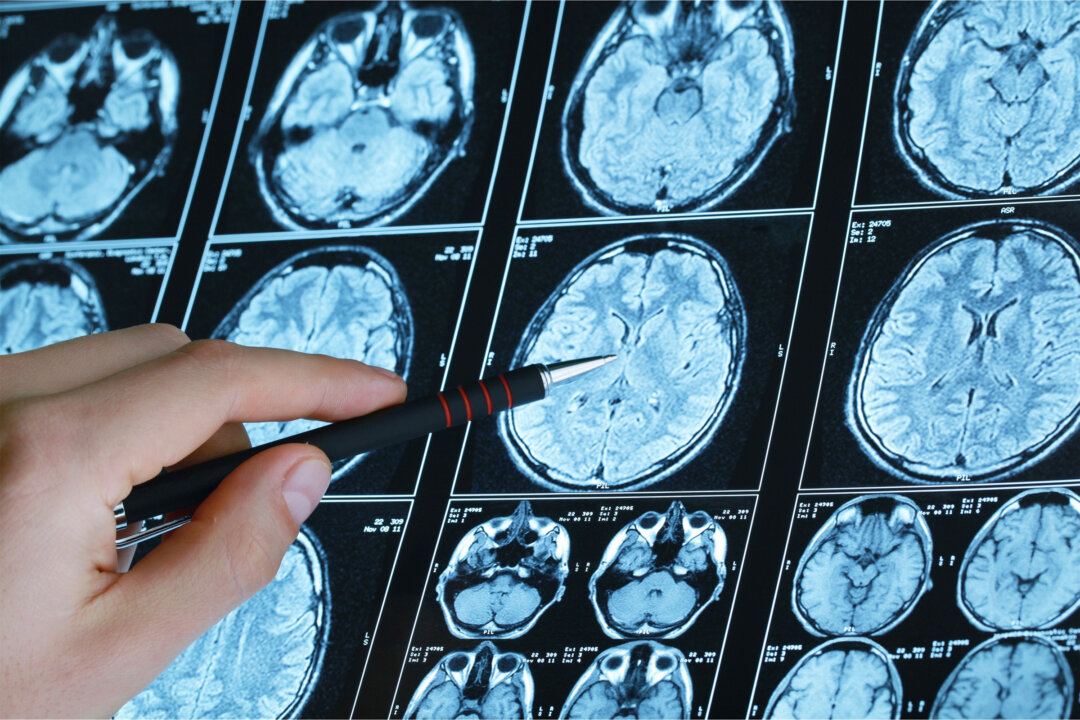
High blood pressure scars the brain’s white matter, changes that appear on MRI scans decades before memory loss. These hidden injuries are among the strongest predictors of dementia.
“High blood pressure sends force into the brain’s smallest arteries,” Prabhakaran said. “They’re not designed to handle it, so they thicken, break, or leak. That leads to silent strokes, white matter damage, even microbleeds—long before memory problems appear.” A silent stroke is one that causes real brain damage but no obvious symptoms at the time.
Nearly 16 percent of dementia cases worldwide—about 9.5 million people—are linked to hypertension, a 2023 analysis found. Warding off dementia by just five years could cut new cases in half, translating to extra years of stronger memory and greater independence.
A Johns Hopkins study of more than 13,000 adults found that having high blood pressure in midlife was linked to faster cognitive decline over the next two decades. Those who kept their numbers in check experienced less decline as they aged.
“That kind of damage can begin years before symptoms show up,” Prabhakaran said. “Treating blood pressure early is about preserving memory and independence later in life.”
A Shift Toward Earlier Action
The cutoffs for high blood pressure have not changed: Below 120/80 is normal, 130 to 139/80 to 89 is stage 1 hypertension, and 140/90 or higher is stage 2. What’s new is how doctors are told to respond when numbers slip into the “borderline” stage 1 range.
The old advice was to “keep an eye on it.” Now the message is to act sooner, since even modest elevations can quietly damage the vessels feeding the heart and brain. Nearly half of U.S. adults already meet this stage 1 definition.
For patients with diabetes, kidney disease, prior stroke, or a 10-year risk above 7.5 percent, drugs may be recommended right away. For others, closer monitoring and a structured follow-up plan replace the old reassurances.
When Lower Isn’t Always Better
Lowering blood pressure isn’t always a win, especially for older adults. A 2020 study found that seniors who struggled to walk 20 feet actually lived longer when their pressure ran a bit higher. While the landmark SPRINT trial showed benefits of stricter targets, it also revealed more kidney injury, mineral imbalances, and fainting in those treated most intensively.
Some physicians, such as Dr. Kenny Lin, associate director of the Lancaster General Hospital Family Practice residency program and an author of the 2022 AAFP Hypertension guideline, say those numbers don’t translate to the real world.
In a typical 15-minute visit, doctors are managing not just blood pressure but diabetes, obesity, sleep apnea, and depression. Following research protocols—patients resting quietly for five minutes on an empty bladder before an automated check—would take up half the appointment.
Even getting patients below 140/90 can be difficult. Pushing them toward 120 or 130 usually requires second or third drugs, raising costs, side effects, and risks from multiple medications. The most common complications are dizziness and acute kidney injury. Kidney function often recovers, Lin said, but not before causing patients and doctors considerable stress.
The gains from driving numbers lower are real but limited, preventing a small number of heart attacks but often at a cost. That’s why some physicians argue that treatment should be tailored, not dictated by a rigid cutoff. Dr. Andy Lazris, a primary care geriatric physician and author of “Curing Medicine,” said guidelines often overlook the complex issues that older patients face.
Taken together, the evidence underscores the need for nuance. Stiffer arteries in later life may require more pressure to keep blood flowing, and treatment must balance brain protection with the risks of falls and fainting that can come with overly aggressive targets to lower blood pressure.
Lifestyle As the 1st Prescription
The guidelines stress that the first prescription for high blood pressure isn’t a pill, but daily habits. Doctors urge patients to manage weight, eat more plants, cut back on salt, stay active, sleep well, ease stress, and limit alcohol.
Even small changes can pay off. Cutting 1,000 milligrams of sodium a day—most of it from processed foods—can lower blood pressure by about five points. Increasing potassium also lowers blood pressure, relaxing the vessels and reducing strain. For the first time, the guidelines recommend potassium-based salt substitutes at home, although they aren’t safe for everyone.
“Patients with kidney disease, and especially diabetics, may have an impaired ability to secrete potassium, and this is further complicated by some of the medications that are recommended,” Dr. Stephen Fadem, a nephrologist and chair of the American Association of Kidney Patients medical advisory board, said in a previous email to The Epoch Times.
Exercise brings some of the strongest returns. A review in Current Hypertension Reports found that regular activity can lower systolic pressure by five to seven points, similar to some drugs. It also boosts circulation and releases brain chemicals that support memory.
Sleep adds its own protection, helping the brain clear Alzheimer’s-linked proteins, while stress management keeps cortisol from damaging blood vessels and cognition.
When lifestyle changes aren’t enough—or when risks are high from the start—medication is added. Most people with readings of 140/90 or higher will need it. For lower-risk patients, doctors recommend three to six months of daily changes first, then drugs if pressure stays above 130/80.
“Exercise and good sleep benefit the brain beyond lowering blood pressure,” Prabhakaran said. “They improve blood flow, reduce inflammation, and protect against long-term brain aging. While lifestyle changes often improve numbers on the cuff, it’s also about overall brain health.”
Tools for the Clinic and Home
The guidelines highlight new tools for prevention. One is the PREVENT calculator, introduced in 2023, which estimates heart disease risk in 10 years and again three decades later, starting at age 30.
Unlike older models, it factors in heart failure along with heart attack and stroke, and uses familiar health measures such as blood pressure, cholesterol, blood sugar, and kidney function—plus age, sex, and even ZIP code. Doctors may soon use it in routine visits to give patients a better sense of long-term risk.
The PREVENT calculator helps doctors tailor risk estimates, and the American Heart Association’s “Life’s Essential 8” gives patients concrete steps—including diet, exercise, and sleep—to lower that risk. Both reflect a turn away from generic advice toward guidance that is more personal and practical.
The guidelines urge doctors to look beyond a single blood pressure reading taken in their office. Home monitors and wearable cuffs that track blood pressure around the clock often uncover hidden problems such as masked or nighttime hypertension. A 2024 meta-analysis found that these out-of-office checks predict cardiovascular risk more reliably than clinic readings.
Checking blood pressure at home works only if patients have support through education or telehealth sessions that help them understand the numbers. A blood pressure cuff on its own, without follow-up from a provider, rarely makes a difference.
The report is cautious about gadgets. Smartwatches and cuffless monitors are too unreliable for clinical use. For now, validated arm cuffs are the standard and should stay at the center of care.
From Numbers to Daily Life
The new targets are clear—few people meet them. Only one in four adults with high blood pressure has it under control, according to the Centers for Disease Control and Prevention, with rushed doctor visits, poor diets, and lost sleep among the reasons.
For patients, the advice is simple: Know your numbers, check them at home, and act even if you feel fine. High blood pressure awareness isn’t just about avoiding stroke or heart attack. Controlling it can help people stay sharp, keep driving, and live independently longer.
“Framing this around brain health may motivate people to take blood pressure more seriously, especially in midlife,” Prabhakaran said. “No one wants to lose independence or quality of life later on. Controlling blood pressure is really a preventive, anti-aging strategy for the brain.”
Too often, he added, people imagine they can wait until they are older, when the threat feels more immediate. “But brain health is about the future we all care about—being able to enjoy life and stay independent in later years,” Prabhakaran said.