Affecting over 32.5 million adults in the United States, osteoarthritis is one of the leading disabling diseases and the most common form of arthritis. It affects the joints, causing wear and tear, inflammation, and pain.
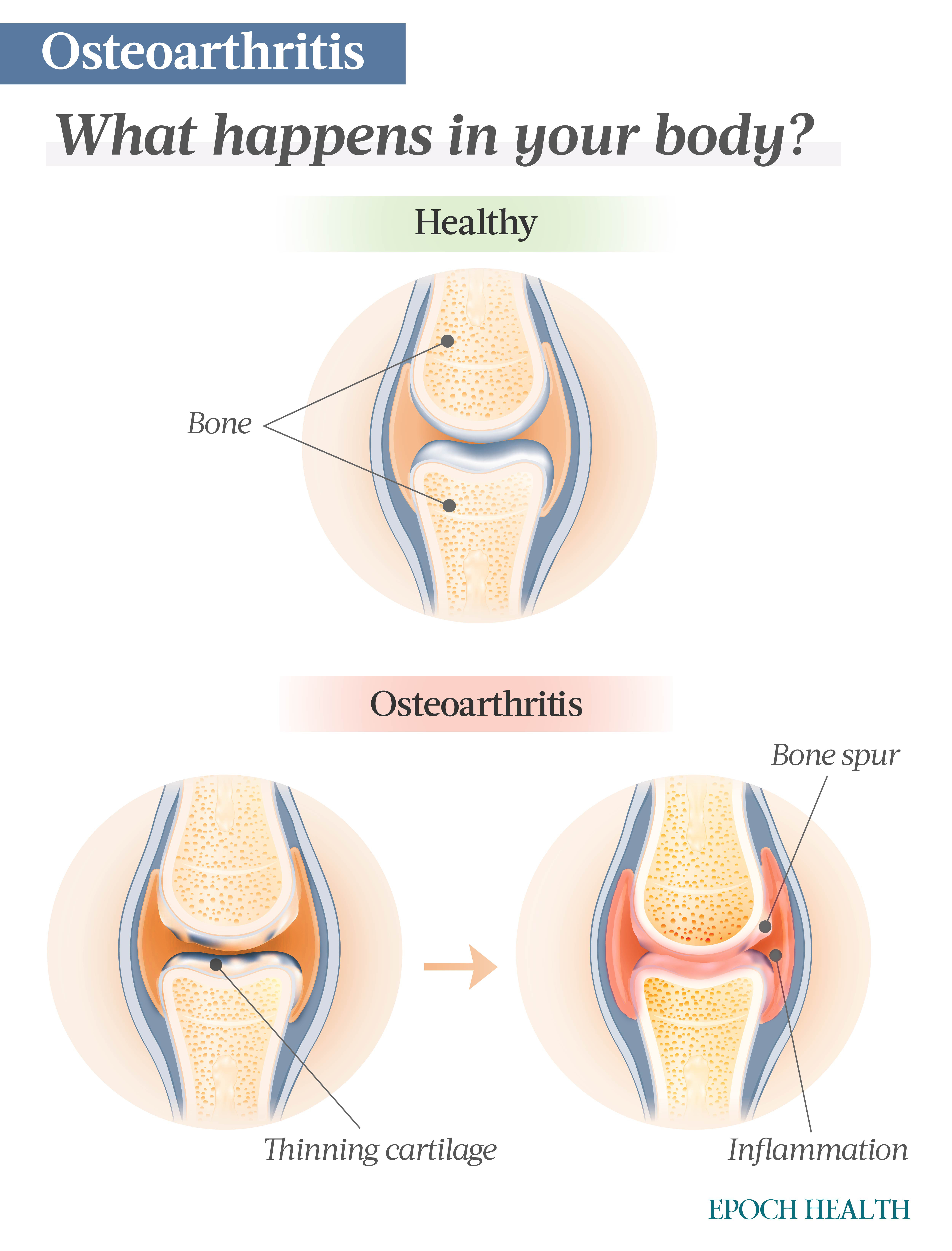
This type of arthritis affects any joint, including the bone, cartilage, ligament, and synovium, the tissue lining the joint. Cartilage is a firm but slippery tissue that cushions the joint, allowing for the joint’s frictionless movement.
The joints most often affected by osteoarthritis are the hands, knees, hips, and spine.
When osteoarthritis affects the spine or hips, bone spurs can form, and disks, which are composed of cartilage, can narrow. In the knees, it deteriorates cartilage, causing the bones to rub together.
[shortcut_anchor id=”anchor_1712780541768″ label=”Symptoms”]What Are the Symptoms and Early Signs of Osteoarthritis?[/shortcut_anchor]
Osteoarthritis has symptoms that differentiate it from other types of arthritis. Symptoms do not arise suddenly; they develop over time. Symptoms may include the following:
- Pain occurring with movement of the joint.
- Stiffness occurring after a time of inactivity.
- Tenderness or discomfort when the joint is touched.
- Inflexibility or a loss of full range of motion.
- Grating sensations with movement.
- Bone spurs, formations of excess bone.
- Swelling around the joint.
- Crepitus, clicking and popping noises when the joint moves.
- Muscle weakness surrounding the joint.
- Buckling, causing the joint to give out.
Symptoms can vary depending on the joint.
Pain is a common symptom among all affected joints. In osteoarthritis of the hip, pain can radiate to the groin, buttocks, or inside the knee or thigh. Pain in the feet typically occurs in the big toe.
The gradual appearance of symptoms can delay diagnosis. Early signs can include aches and pains in the joints, especially toward the end of the day or at night, stiffness, and new cracking or popping sounds, often in the knees.
[shortcut_anchor id=”anchor_1712780551254″ label=”Stages”]What Are the Stages of Osteoarthritis?[/shortcut_anchor]
Osteoarthritis progresses in four stages. Some staging begins at pre-osteoarthritis (stage 0) and ends at stage 3; others consist of stages 1 through 4. Ultimately, these stages lead to an overgrowth of bone to stabilize the joint. Stages include the following:
- Stage 0 is pre-osteoarthritic. This stage may last for years, as osteoarthritis is a slow degenerative disease. People are symptom-free during this stage.
- Stage 1 is when the cartilage begins to break down. It starts with the overproduction of enzymes, resulting in a breakdown of the cartilage matrix. Minor bone spurs may be visible on X-rays in this stage. Pain is minimal, with some stiffness.
- Stage 2 is when joint cartilage begins to fray and split. The splitting throws pieces into the synovial fluid, and the joint takes on structural damage. At this stage, regular activity may cause pain. Joint spacing begins to narrow.
- Stage 3 initiates the chronic inflammatory response in the synovium. The synovium immune cells release multiple inflammatory proteins that directly attack the cartilage. Inflammation is chronic at this point, along with constant pain and stiffness. More and more prominent bone spurs are present.
[shortcut_anchor id=”anchor_1712780558854″ label=”Causes”]What Causes Osteoarthritis?[/shortcut_anchor]
The cause of osteoarthritis depends on its type. There are two types of osteoarthritis: primary and secondary.
Primary
Primary osteoarthritis, the more common of the two, is the deterioration of cartilage at the joint without an apparent reason. It is typically attributed to age and long-term wear and tear.
Healthy people’s bodies produce degradative and synthetic enzymes to maintain cartilage volume.
In individuals with osteoarthritis, the degrading enzymes are overproduced, resulting in net degradation.
Deterioration of cartilage begins the cascade of osteoarthritis events. The ends of the bone begin to thicken and harden, forming bone spurs, which make joint movement difficult. Bits of bone and cartilage can break off, leading to the growth of cysts in the bone.
Osteoarthritis’ progression is commonly slow. However, certain events can accelerate the progression. A contributor to the faster progression of osteoarthritis is musculoskeletal abnormalities.
Secondary
Secondary osteoarthritis is caused by another condition. A deformity, infection, injury, or other disease can result in the deterioration of joint cartilage.
Since environmental factors cause secondary arthritis, they can sometimes be addressed. A person’s occupation, muscle strength, weight, and diet can be modified. Other factors needing more professional intervention include unbalanced sex hormones, decreased bone density, and prior joint injuries. These can all lead to malalignment.
Malalignment is when the bone or joint does not align. Muscles support the joint by helping it stay aligned. Weak muscles no longer support the joint and may result in malalignment, accelerating osteoarthritis progression. Recently there has been evidence that correcting malalignment may reverse some cartilage damage.
[shortcut_anchor id=”anchor_1712780609447″ label=”Risk Factors”]Who Is at Risk of Osteoarthritis?[/shortcut_anchor]
Several factors can put you at risk for osteoarthritis. Those you cannot change include the following:
- Age: The risk for osteoarthritis increases with age. Over 50 percent of people 65 and older have osteoarthritis.
- Sex: Women are disproportionately more likely to have osteoarthritis, but the reason is unknown.
- Family history: Those with a family history are more likely to develop osteoarthritis.
- Genetics: Conditions like Ehlers-Danlos syndrome can contribute to osteoarthritis. This condition makes connective tissue weak, thus, affecting joints. It is incurable.
- Bone deformities: People born with bone deformities have an increased risk of osteoarthritis.
- Certain metabolic diseases: Metabolic disorders like hemochromatosis (too much iron in the body) can increase the risk of developing osteoarthritis.
- Race: According to the U.S. Centers for Disease Control and Prevention (CDC), some Asian people may be less at risk than others.
Modifiable factors include the following:
- Obesity: Obesity contributes to developing osteoarthritis by adding joint stress and inflammation.
- Joint injuries: Sports injuries or any other joint injury, regardless of how long ago they occurred, can increase the chances of developing osteoarthritis.
- Occupation and/or repetitive stress: Repeated stress on a joint or repetitive movement can increase your risk of osteoarthritis.
Although osteoarthritis is most common among older people, younger people who have had a torn ACL or meniscus are more at risk of developing osteoarthritis.
[shortcut_anchor id=”anchor_1712780617390″ label=”Diagnosis”]How Is Osteoarthritis Diagnosed?[/shortcut_anchor]
Diagnosis of osteoarthritis starts with self-assessment and symptom monitoring.
Self-assessment is as easy as journaling about how you feel, observing how your joints behave, and when symptoms occur and how long they last. Sharing the journal with a health care professional can help you receive personalized treatment and address symptoms early.
Joint pain is one of the most common symptom that brings people to see their primary health care provider. You can expect the provider to review your history of symptoms and perform a physical exam. The provider may order tests depending on your history and physical findings to assist in diagnosis. These can include the following:
- X-rays, which can show changes in the bone caused by osteoarthritis or other joint damage.
- Magnetic resonance imaging (MRI) to provide a better view of the joint cartilage and other tissues.
- Aspiration of joint fluid to identify other causes of joint pain, like infection or gout.
- Blood tests that rule out other causes of the symptoms.
After seeing your primary care provider, you may see other specialists depending on the progression of the disease and your treatment plan.
[shortcut_anchor id=”anchor_1712780627677″ label=”Complications”]What Are the Complications of Osteoarthritis?[/shortcut_anchor]
Osteoarthritis comes with many complications, including:
- Anxiety and depression.
- Sleep disturbances due to pain.
- Difficulty exercising, which can affect weight and wellness.
Other complications of osteoarthritis arise for different reasons, like medication side effects and reduced mobility. These complications include the following:
- Overweight and obesity.
- Diabetes.
- Heart disease.
- High cholesterol.
- High blood pressure.
- Falls.
- Fractures.
- Dizziness from osteoarthritis medication.
- Social isolation, resulting in poorer quality of life.
[shortcut_anchor id=”anchor_1712780634974″ label=”Treatments”]What Are the Treatments for Osteoarthritis?[/shortcut_anchor]
While the rate of osteoarthritis progression may be slowed, the damage already done by the disease cannot be reversed. At this point, symptom management becomes the focus.
As you learn about your body’s response to osteoarthritis, you will discover ways to help you address your symptoms. Educating yourself is the first step to understanding osteoarthritis and how you can manage symptoms.
Your primary health care provider may also refer you to specialists to create your treatment plan. These specialists include the following:
- Rheumatologists focus on treating arthritis and other conditions related to arthritis.
- Dieticians can help you reach your nutritional and weight goals.
- Nurse educators can answer questions about lifestyle changes or how to manage symptoms.
- Physical therapists assist in improving joint function and can teach you how to exercise, allowing you to continue therapy at home.
- Occupational therapists teach you how to move your joints correctly to protect them and minimize pain.
- Physiatrists can be physical, medicine, and rehabilitation specialists who help supervise exercise programs.
- Chiropractors consider the relationship between the body’s structures. Their primary focus is on the spine.
- Psychologists can help with the complications of osteoarthritis that affect your mental health.
- Orthopedic surgeons specialize in the surgical treatment of bone and joint diseases. You may not see this specialist until late in the disease state.
Working as a team, your care providers organize your treatment plan, which may include different therapies. These can be pharmacological, nonpharmacological, and surgical.
1. Nonpharmacological Treatment
Nonpharmacological management of osteoarthritis symptoms involves therapies other than pharmaceuticals.
- Lifestyle: These modifications should include stretching, a nutritious diet, weight loss if necessary, and exercise. Exercises should include strengthening, range-of-motion, aerobic, cardio, and balancing exercises.
- Physical and occupational therapy: Physical and occupational therapists can help you strengthen and protect your joints by teaching you specific exercises to stabilize joints to minimize pain and instructing you on proper joint movement.
- Assistive devices: Assistive devices can strengthen weak joints by providing external support. They may also assist with mobility and stability when walking. Assistive devices include crutches, canes, knee braces, and shoe inserts.
2. Pharmacological Treatment
Managing osteoarthritis with medications can be as simple as taking over-the-counter (OTC) pain medication. When OTC medication is ineffective, health care providers may prescribe other medicines.
OTC Medication
OTC medications can be oral pain medications or topical creams. They include the following:
- Analgesics: Pain relievers that include acetaminophen.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs like ibuprofen and aspirin relieve pain and inflammation.
- Counterirritants: Topical creams like lidocaine provide warming, cooling, or mildly irritating effects to reduce one’s attention to the painful area.
The benefits of topical creams require regular use. These creams may have side effects, such as itching, burning, and rash. You should stop taking them and notify your health care provider if you experience any side effects.
Prescription Medication
If OTC medications are ineffective, your health care provider may prescribe the following prescription medications:
- Corticosteroids, which are anti-inflammatory drugs.
- Antidepressants like duloxetine.
- Anti-seizure medication like pregabalin, which is now approved by the U.S. Food and Drug Administration (FDA) for the treatment of osteoarthritis. Its mechanism is likely due to its effect on central pain pathways.
- Injectable corticosteroids for inflammation.
- Platelet-rich plasma (PRP) injections. This therapy is not approved by the FDA, and research is mixed on its effectiveness.
- Hyaluronic acid injections. Hyaluronic acid exists naturally in the human body and helps cells retain moisture. While it may offer relief for people with mild to moderate osteoarthritis, the results of its efficacy have been controversial (pdf).
3. Surgical Treatment
A few types of surgeries may help treat osteoarthritis, especially in severe cases. Surgical interventions include the following:
- Joint replacement: When a joint has become too damaged, the pain becomes intolerable and movement restricted; in this case, a joint replacement may be in order. Replacement of the hip and knee joints has a 90 percent success rate, and the prosthetic joint has a life expectancy of about 10 to 15 years. Because of this short lifespan, some people may need multiple joint replacements.
- Arthroscopy: Arthroscopy involves inserting a camera into a small incision to evaluate joint damage. Repairs can also be made this way.
- Osteotomy: In an osteotomy, a surgeon cuts bone(s) and realigns the joint. Osteotomy of a limited portion of the knee adjusts the joint alignment and takes pressure off the damaged cartilage.
[shortcut_anchor id=”anchor_1712780651494″ label=”Mindset”]How Does Mindset Affect Osteoarthritis?[/shortcut_anchor]
Mental health and its repercussions can affect osteoarthritis progression and, inversely, can also be a complication of osteoarthritis.
Performing daily activities can be difficult for people with osteoarthritis, leading to a sense of inadequacy and loss. These feelings can worsen into depression. When in a depressive state, people may stop caring for themselves and require the assistance of others. People with arthritis must be aware of their mental health and get help when necessary.
In a small study of 94 people with osteoarthritis, over half (58.5 percent) had a mental health condition. These conditions included:
- Somatic symptoms disorder.
- Obsessive-compulsive disorder.
- Depression.
- Anxiety.
- Aggression.
- Phobia.
- Paranoid psychosis.
According to the study, these mental health conditions paired with osteoarthritis tend to appear more often in those under 40. This may be due to newer diagnoses among that age group, as patients haven’t had as much time to learn how to manage the condition. It could also be that an osteoarthritis diagnosis simply takes a heavier mental toll on younger patients.
Anxiety and depression are common complications of osteoarthritis. People with these conditions may experience more intense pain, have more hospital visits, take more medications, and have less favorable outcomes, resulting in a lower quality of life.
A positive outlook can increase the quality of life of those with osteoarthritis. Instead of focusing on their disabilities, positive people focus on their strengths, giving them a more accurate look at themselves and how they can be active community members.
[shortcut_anchor id=”anchor_1712780662670″ label=”Natural Approaches”]What Are the Natural Approaches to Osteoarthritis?[/shortcut_anchor]
Complementary and alternative therapies might be used in conjunction with treatments recommended by your health care provider. Discuss with your provider what is best for you when considering these therapies.
1. Acupuncture
Acupuncture uses tiny needles placed in certain areas to minimize pain and other conditions. Some research shows that acupuncture can help with osteoarthritis pain, especially in the knees. The reason it works is unclear, but some researchers believe the needles cause the release of natural pain relievers in the body.
2. Supplements
Some herbal and dietary supplements may manage osteoarthritis. Herbal supplements are not regulated. Discuss their use with a health care provider before adding them to your treatment routine. Supplements used to manage osteoarthritis include the following:
- Glucosamine with chondroitin sulfate: This supplement may decrease knee osteoarthritis pain with minimal side effects. However, avoid it if you have a shellfish allergy. Diabetics should be aware that glucosamine may also raise blood sugar. Do not take it if you’re on anticoagulant or anti-platelet medication, as chondroitin can interfere with these. A paper in Australian Prescriber claims glucosamine has the same effects as a placebo.
- Frankincense (Boswellia serrata): This botanical has anti-inflammatory, analgesic, and anti-arthritic properties. One systematic review and meta-analysis found frankincense extract improved pain, stiffness, and joint function after one month of use. Another study found it increased physical function without serious side effects.
- Curcumin: Curcumin, the bioactive compound in turmeric, has anti-inflammatory and antioxidant effects due to its inhibiting the production of inflammatory mediators. One study found it safer and has fewer adverse effects than the NSAID diclofenac. It was also shown to reduce knee pain with minimal side effects.
- Aloe vera: One review in the British Journal of Community Nursing found that oral Aloe vera may effectively treat osteoarthritis pain due to its anti-inflammatory effects. It also appears to help prevent gastrointestinal irritation due to NSAID use.
- Fish oil: Fish oil contains anti-inflammatory fatty acids that may be beneficial in minimizing osteoarthritis inflammation.
- Vitamin D: Among other things, vitamin D promotes the health of bones and cartilage.
- Vitamin K: This vitamin assists with bone formation. Deficiency of vitamin K has been associated with knee osteoarthritis.
- Topical capsaicin: Derived from chili peppers, this cream can relieve osteoarthritis pain. Be sure to wash your hands after applying it so you don’t accidentally spread it to sensitive areas.
3. Heat and Cold Therapies
Applying heat or cold may help the inflammation in a joint and relieve pain. Heat increases blood flow to the joint, providing nutrients. It also increases pain tolerance and improves flexibility.
Cold therapy affects the nerves around the joint. It temporarily numbs them, providing relief. It also helps alleviate joint inflammation.
4. Mind-Body Therapies
Other forms of therapy may involve using your mind in tandem with your body to help relieve osteoarthritis symptoms. These may include exercises or techniques to calm and relax you, such as the following:
- Support groups may offer support and help you cope with living with osteoarthritis.
- Deep breathing can help calm you and ease tension.
- Meditation involves breathing techniques and can help with focus and relaxation.
- Yoga can help you maintain flexibility, strength, and balance.
- Tai chi, a gentle martial art involving meditative movement, can help strengthen muscles and improve your range of motion.
- Music therapy can help ease anxiety and depression.
[shortcut_anchor id=”anchor_1712780685567″ label=”Prevention”]How Can I Prevent Osteoarthritis?[/shortcut_anchor]
Osteoarthritis is the result of the regular use of your joints. Over time, joints will become worn and arthritic. You cannot completely prevent wear and tear from joint use. We must use our joints regularly to keep them strong and to keep the rest of our bodies as healthy as possible. However, you can reduce stress on your joints.
Identify any modifiable risk factors you may have, and make the following changes:
- Be physically active: As mentioned, this has many benefits for osteoarthritis but can also help you prevent the condition.
- Lose weight if you are overweight: This is tremendously helpful. The benefits of weight management to minimize the risk of osteoarthritis are the same as those that help people live with it.
- Attend regular doctor appointments: Being active in your treatment plan keeps you informed of changes and allows you to share updates with your health care provider.
- Eat a healthy diet: Green leafy vegetables are a good source of vitamin K. Oily fish like salmon provide omega-3 fatty acids. Olive oils should replace seed oils, such as corn and sunflower, which may cause inflammation. Fruits and vegetables are high in fiber, and fiber may lower inflammation.
- Avoid joint injury: Repetitive actions and stress on the joints can aggravate natural wear and tear, putting you at risk of osteoarthritis.



