Advancements in artificial intelligence (AI) could provide breakthroughs in the way that we detect breast cancer and evaluate breast cancer risk.
A recent Swedish study found that AI was able to detect 20 percent more breast cancer than experienced radiologists—in addition to cutting their mammography reading workload by more than 40 percent. The study suggests that AI could be a useful tool for breast cancer detection as well as help doctors and radiologists to do their jobs more effectively.
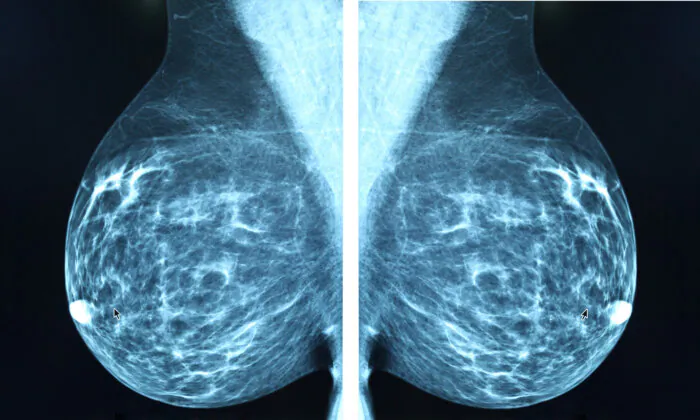
The study—a randomized, controlled, population-based trial published in The Lancet Oncology—looked at 80,033 mammograms of women in Sweden. The participants, ages 40 to 80, were split into two groups. From April 2021 to July 2022, the mammograms of one group of women were read by AI before being analyzed by a radiologist, and the second group had their mammograms read by two radiologists without the use of AI.
The group of women who had their mammograms read by the AI as well as a radiologist had 20 percent more cancers detected than the group whose mammograms were read by two radiologists.
“In our trial, we used AI to identify screening examinations with a high risk of breast cancer, which underwent double reading by radiologists. The remaining examinations were classified as low-risk and were read only by one radiologist. In the screen reading, radiologists used AI as detection support, in which it highlighted suspicious findings on the images,” Kristina Lang, the study’s lead researcher, wrote in an article about the study on the Lund University website. Ms. Lang is an associate professor in diagnostic radiology at the university, as well as a consultant at Skane University Hospital.
The study found that in the AI group, 75 percent of cancers detected were invasive and 25 percent were in situ. Among those who had their mammograms analyzed by two radiologists (considered the control group), 81 percent of cancers detected were invasive and 19 percent were in situ.
Carcinoma in Situ
Carcinoma in situ happens when cells may look cancerous under the microscope but are localized and haven’t spread beyond their source. The words “in situ” mean “in its original place.” Carcinoma in situ is considered a stage zero, or noninvasive cancer. The in situ cells aren’t malignant or cancerous, but they can sometimes become cancerous and spread from their original location.
Carcinoma in situ can occur anywhere in the body, but there are two types associated with the breast: ductal carcinoma in situ (DCIS) and lobular carcinoma in situ (LCIS).
Ductal carcinoma in situ occurs when cells are growing in the milk ducts of the breast, and lobular carcinoma in situ means that they’re growing in the lobules of the glands in the breast that produce milk.
DCIS turns into cancer in only about 20 percent of cases, and about 60,000 people are diagnosed with DCIS each year in the United States.
It’s important that women understand the meaning of carcinoma in situ—and especially DCIS and LCIS, which pertain to the breast—in order to decide whether they would prefer it to be treated or not. Many doctors may not fully explain DCIS and LCIS, which may cause women to have treatments that aren’t necessary. Detecting these types of cancer via mammography lets doctors and oncologists pay attention to them to ensure that the cells don’t spread from their origin and develop into breast cancer in the future.
Helped to Decrease Workload
The study also concluded that the mammogram-reading workload was reduced by 44 percent using AI. To put that in perspective, the AI-supported group had 46,345 mammograms and, according to Ms. Lang, radiologists read an average of 50 screening examinations per hour. The researchers estimated that the AI reduced the time that it would have taken radiologists to read that number of screenings by about five months.
In Sweden, each breast screening examination is read by two breast radiologists—called a double reading—in order to ensure accuracy. However, problematically, there’s a shortage of breast radiologists in Sweden and elsewhere. Perhaps in the future, the addition of AI can help to alleviate some of the work hours involved in reading breast screening examination results.
AI Had No Effect on False Positives
“We found that using AI resulted in the detection of 20 percent (41) more cancers compared with standard screening, without affecting false positives. A false positive in screening occurs when a woman is recalled but cleared of suspicion of cancer after workup,” Ms. Lang wrote.
False positives are a concern with mammography screening programs. The chance of having a false positive after a single mammogram is thought to be about 7 percent to 12 percent, and is more common in younger women and women with dense breasts (about 40 percent of women). The chances of receiving a false positive result increases over time, however, with the risk after 10 years of annual mammograms climbing to 50 percent–60 percent.
Doctors and scientists are urgently searching for more effective ways to detect breast cancer and predict breast cancer risk, as incidence rates are increasing at a rate of 0.5 percent a year. Breast cancer now accounts for about 30 percent of all new cancer diagnosed in women in the United States annually and is now the most common cancer in the world, accounting for 12.5 percent of all new cases of cancer worldwide annually.
Other Studies Using AI to Detect Breast Cancer
Other studies have also explored ways that AI can help to identify breast cancer.
One study showed that AI is better at predicting breast cancer risk than standard clinical risk models. The study used mammograms that were assessed with five AI algorithms, and all were able to predict five-year breast cancer risk better than the standard models used to determine risk. The algorithms identified both missed cancers and features in breast tissue that help to predict future cancers. The study also found that the combination of the AI algorithms and the risk models further improved breast cancer prediction.
An article in Becker’s Hospital Review states that Hungarian physicians are using AI that’s able to detect breast cancer four years before it develops. The technology is called computer-assisted detection, and with it, the AI can identify areas on a mammogram that radiologists and physicians should inspect more closely.
MIT’s computer science and artificial intelligence lab has also developed an AI prediction model that’s able to foresee the development of breast cancer up to five years in advance by using a patient’s mammogram. The algorithm was trained using more than 200,000 exams and was significantly more accurate than previous methods in predicting cancer risk and identifying groups that were high risk. A resulting study was published in Science Translational Medicine.
A recent study published in Radiology sought to assess how effective AI could be for detecting breast cancer. Using a commercially available AI algorithm, researchers compared the AI with 552 human readers of screening mammograms. The study found that the AI performed as well as human readers in detecting breast cancer.
The National Cancer Institute estimates that about 20 percent of breast cancers are missed using mammography. Perhaps the addition of AI algorithms may be able to augment breast cancer detection and increase women’s odds of survival.
So what does the future hold for using AI for breast cancer screening? In a statement on the Lund University website about the Swedish study, Ms. Lang notes that screening is a complex process and states:
“The balance between benefit and harm must always be taken into account. Just because a screening method finds more cancers does not necessarily mean it’s a better method. What’s important is to find a method that can identify clinically significant cancers at an early stage.
“However, this has to be balanced with the harm of false positives and the overdiagnosis of indolent cancers. The results from our first analysis show that AI-supported screening is safe since the cancer detection rate did not decline despite a substantial reduction in the screen-reading workload.”
A planned analysis of interval cancers—cancers that show up suddenly between regular screenings and are often aggressive—will show whether AI-supported screening also leads to a more accurate and effective screening program, according to Ms. Lang.