When Crystal Doyle’s 7-year-old tumbled out of bed one night, she was groggy, nauseated, and later vomited—by morning, swelling around one eye set off alarms. Doyle feared a concussion but couldn’t tell whether it was serious or just another fall. With a high-deductible health plan, she weighed what was best for her daughter against what her family could afford.
“Walking into urgent care is a couple hundred dollars, but the ER is over $1,000,” Doyle said. “Of course, if it were something obvious, money wouldn’t even be on your mind—you’d just go.”
Millions of families face the same gamble. A child spikes a fever at 9 p.m. A grandparent feels chest tightness on a Saturday. A teenager sprains an ankle over a holiday weekend. In those moments, with no doctor to call and the clock ticking, families must answer a question the health care system has never made clear: Do you wait until Monday to call your doctor, head to urgent care, or go straight to the emergency room?
The Price of Uncertainty
In theory, the system has three lanes: the ER for life-threatening crises, urgent care for the gray zone between routine and critical, and primary care for everything else. In practice, those lines often blur.
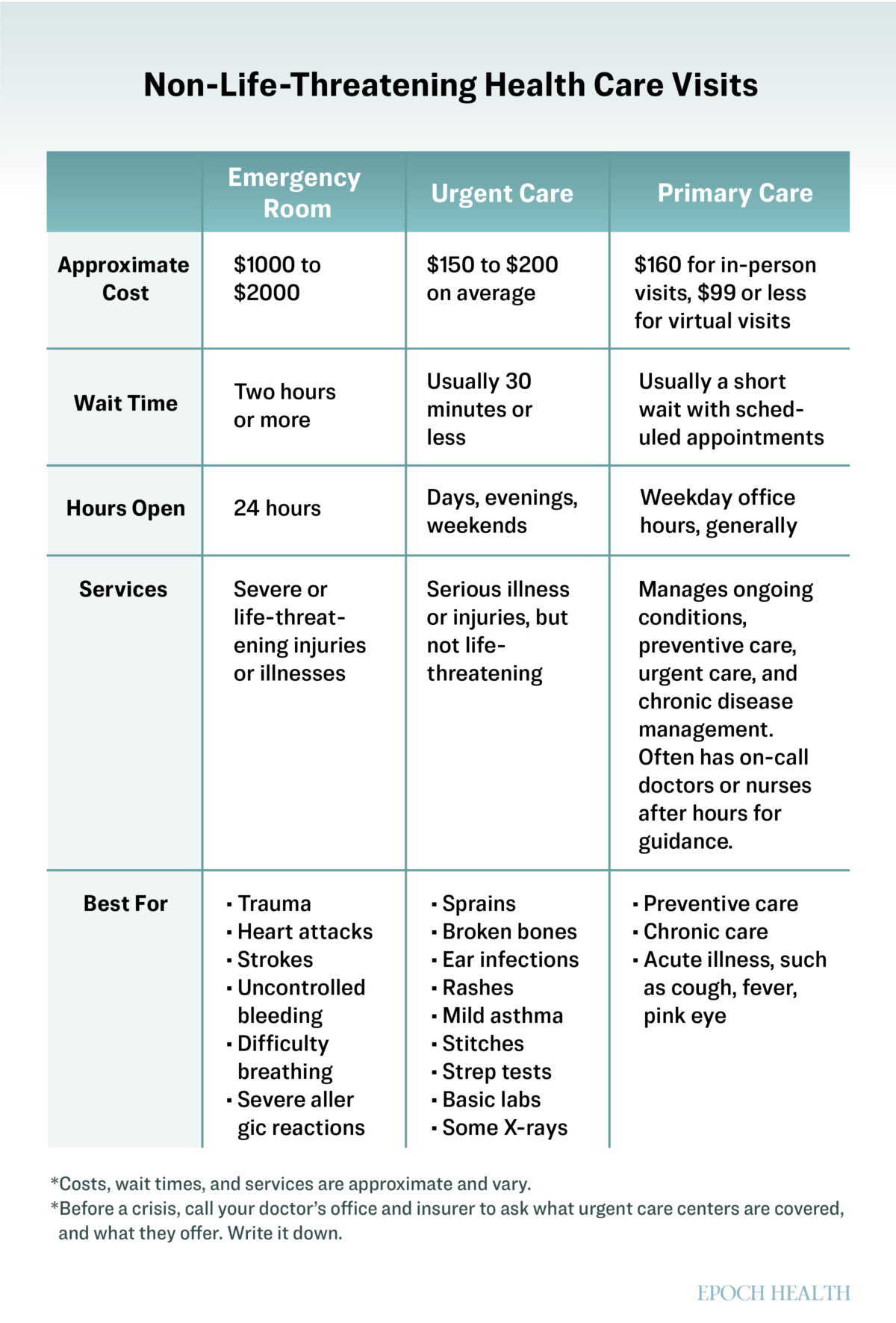
Emergency departments are always open, but they’re the most expensive entry point into care. A typical visit runs about $1,700, which is 10 times the cost of urgent care. In 2021, 107 million ER visits added up to $80 billion nationwide, and analysts estimate that two-thirds of cases among privately insured patients could be safely treated elsewhere.
For families with high-deductible plans—insurance that requires paying thousands out of pocket before coverage begins—that decision can feel like a gamble.
“It’s hard when it’s not obvious if you need to be seen and you have a high deductible,” Doyle said.
In one national survey, 38 percent of Americans said they delayed care because of cost, even when they thought they needed it.
Money isn’t the only factor. People also weigh whether they can get a ride, how long they’ll wait, what their insurance will cover, and—perhaps most of all—how dangerous their symptoms really are.
None of the doors is a perfect fit. Primary care, meant to anchor the system, often closes after hours and on weekends—exactly when most health scares happen. Urgent care fills some of the gap but varies widely in capability: One clinic may set a fracture; another may only wrap and refer. That leaves the ER, built for true emergencies, functioning as a default catchall for everyone who has nowhere else to go.
All of those point to a bigger problem, Dr. Alexander Janke, an emergency physician at the University of Michigan, told The Epoch Times.
“Acute care access is fundamentally broken in the U.S.,” he said.
Knowing the system is broken doesn’t help much at 10 p.m. when someone is sick or hurt. Here’s what to know so you can make the right call in the moment.
The Emergency Room
Emergency departments exist for life-or-death moments—chest pain, shortness of breath, sudden weakness or numbness, confusion, trouble speaking, uncontrolled bleeding, or major head trauma. These symptoms can worsen within minutes and may signal a heart attack, stroke, internal bleeding, or brain injury.
The ER is the only setting with 24-hour imaging, labs, surgical teams, and specialists on call. Its “one-stop access” means a patient with chest pain can get blood tests, an electrocardiogram, and imaging and see a cardiologist within hours—care that could take days or weeks to coordinate elsewhere.
“The biggest misunderstanding is that patients expect us to determine the exact cause of their problem,” Dr. Jeffrey Druck, vice chair of emergency medicine at the University of Utah, told The Epoch Times. “We’re not there to figure out exactly what is causing your problem. We’re there to make sure it’s nothing life-threatening.”
Walking out without a definitive diagnosis, he said, is often a good sign.
“It usually means nothing life-threatening was found, and the next step is to follow up with your primary-care physician,” he said.
Most ER patients fall into that category. According to federal data, only about 14 percent of visits lead to hospital admission. Many are what physicians call “rule-outs”—visits that end when a major crisis is excluded.
Still, the ER’s efficiency can make it a magnet for problems better handled elsewhere.
“It’s incredibly effective care, but often the wrong setting,” Dr. Brad Frazee, an emergency physician at the University of California–San Francisco and Alameda Health System, told The Epoch Times. “A patient with a swollen knee might get an X-ray, MRI, and an orthopedic consult all in one night. It’s great medicine, but it’s expensive medicine.”
That expense varies. For some privately insured patients, emergency care triggers high deductibles and four-figure bills—for others, it’s covered with only a co-pay.
“Ironically, once you’re in the door, it’s carte blanche—no prior authorization issues,” Frazee said. “And patients know that.”
Adding to the confusion are freestanding emergency departments—facilities that look like urgent care clinics but operate as full-service ERs with 24/7 hours, advanced imaging, and board-certified physicians. Their numbers have surged, from 1 percent of U.S. ERs in 2001 to 12 percent in 2017. Waits are often shorter, but bills match those of hospital ERs—something many families don’t realize until the invoice arrives.
Urgent Care
Urgent care centers were built for the gray zones: a sprained ankle on Saturday night, a toddler’s ear infection at 8 p.m., a cut that needs stitches but not an ambulance.
That’s what Doyle thought when she walked in with her daughter’s head injury. Urgent care felt like the safe middle ground, until staff took one look and sent them to the ER.
“I’m never sure exactly what urgent care does or doesn’t do,” she said.
The appeal is speed and price. An urgent care visit averages $150 to $200—about one-tenth the cost of an ER visit—and waits are usually less than an hour. Many clinics post real-time wait times, stay open on evenings and weekends, and let patients reserve a spot online.
However, they are not miniature emergency rooms. Most lack CT or MRI scanners, and anyone with chest pain, uncontrolled bleeding, or major head trauma will be redirected to the ER. Services also vary widely. One clinic may set a fracture, and another may only wrap and refer; some run in-house labs, and others ship tests away. Families often learn the limits only after they walk through the door.
Yet the lines between the two aren’t always clear.
“You see an 80-year-old with chest pain on the urgent care schedule and think, ‘That’s inappropriate—I’ll have to send them straight to the ER,’” Frazee said.
But many cases turn out to be low-risk—muscle strain, mild reflux, anxiety—and can be safely evaluated if the urgent care has on-site testing and a way to coordinate rapid follow-up.
That’s a big “if.” Many urgent care centers don’t have those resources, so doctors say the safer rule is simple: When in doubt—especially with new or severe chest pain—go to the emergency room.
Despite their limits, urgent care clinics play a vital role in easing the burden on hospitals. Where new centers open, nonemergency ER visits drop by nearly 17 percent—the equivalent of dozens fewer patients each day in a busy department. That can mean shorter waits for true emergencies and fewer families stuck in crowded waiting rooms.
Primary Care
Primary care is the system’s backbone. These are the doctors who know your history, your risks, and your priorities in a way no urgent care physician ever will.
Continuity is its strength. Patients who maintain a steady relationship with a primary care physician live longer, are hospitalized less often, and spend less overall on health care. A 2023 review published in the Annals of Family Medicine examined 83 studies and found that greater continuity was linked to significantly lower costs and more appropriate use of services in nearly 70 percent of cases. That connection can mean the difference between prevention and crisis.
Access is the weakness. Appointments for nonurgent issues can take days or weeks, and most offices are closed on nights and weekends.
“Clinics are built on scheduled care,” Frazee said. “Their ability or willingness to see patients on short notice for unscheduled care is limited or nonexistent.”
That is why so many patients end up in urgent care or the ER for problems that could have been handled earlier. Still, primary care is where ongoing issues should be managed before they become emergencies. For chronic conditions, preventive screenings, or new symptoms that aren’t urgent, your doctor’s office is the right first call. Some practices keep an on-call doctor or nurse who can guide you after hours, and many insurers run 24-hour nurse lines.
Why Patients Keep Choosing Wrong
On paper, the rules seem clear, but in practice, patients make these choices under pressure.
A 2024 PRiMER study found that most people who went to the ER did so not because they believed they were in danger, but because it was the fastest path to care. They knew it was costly, crowded, and impersonal, but still more accessible than waiting days for an appointment or test results.
Fear compounds the impulse. Families often head to the ER “just in case,” worried that mild symptoms could hide something catastrophic. Researchers have called such behavior an “existential fear of the unknown.” People worry about wasting resources, but they fear that the greater mistake is waiting too long.
Frazee said he sees patients err in both directions.
“It cuts both ways—left to their own devices, patients will both catastrophize and minimize,” he said.
In other words, the danger isn’t that patients always overreact—it’s that they’re being asked to judge risk without the tools to do it.
How to Decide in the Moment
Doctors say the best defense is to have a plan before a crisis. A few rules of thumb:
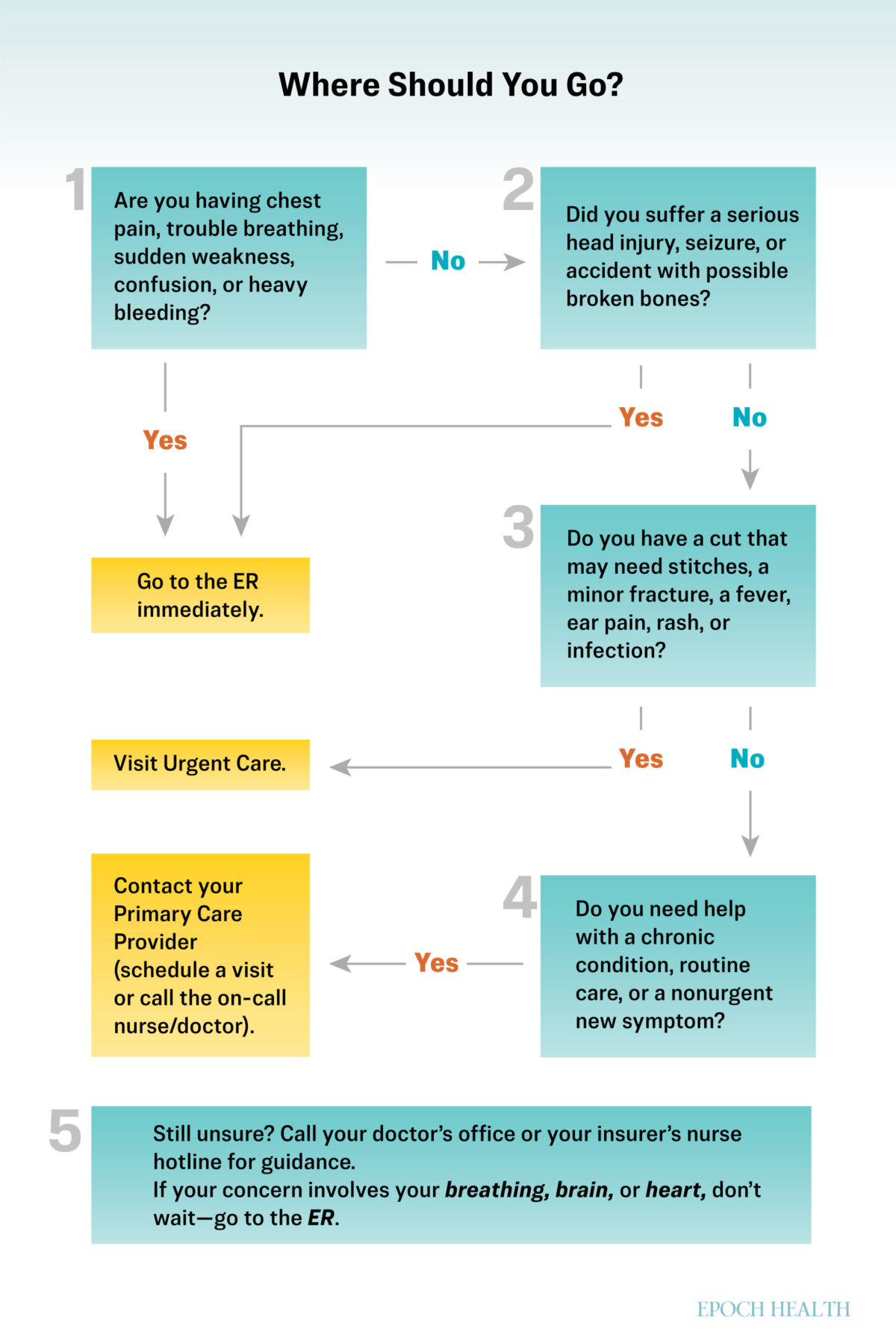
- Watch for Red Flags: Chest pain, trouble breathing, sudden weakness, confusion, uncontrolled bleeding, or a major head injury—go straight to the ER or call 911.
- Think Urgent, Not Life-Threatening: Sprains, cuts that may need stitches, fevers, ear infections, and mild asthma flares belong in urgent care. Call ahead if you’re unsure what a clinic can handle.
- Lean on Primary Care: For ongoing issues or new but nonurgent symptoms, your doctor’s office is the best place to start. Many practices keep an on-call nurse or doctor after hours.
- Use What’s Available: Many insurers and health systems run 24-hour nurse lines or offer virtual urgent care.
- Know in Advance: Find out what services your local urgent care offers, check what your insurance covers, and know how to reach your doctor after hours. The best decisions are not made at midnight in a panic.
For Doyle, the scan was clear, and her daughter was fine. The relief was worth the detour, although the bills lingered. What stayed with her most was the uncertainty—never knowing in the moment whether she was overreacting or not doing enough.
“Next time I’d call first, and I’d go straight to the ER for anything head-related,” she said.
What’s Next: Knowing where to go for treatment in the moment is only half the battle. Once the tests come back, the real work begins—making sense of what “normal” or “abnormal” truly means for your health. Our next article shows how to read your results, spot the gray zones, and ask the right questions when numbers don’t tell the whole story.



