For decades, scientists have wondered whether changing the way we think could actually reshape the brain. Now, a recent study offers compelling evidence, capturing the first images suggesting that psychotherapy, through mental effort alone, may lead to real structural changes in the brain.
For people living with depression, the research points to a deeper way that therapy may help—by rebuilding the brain itself.
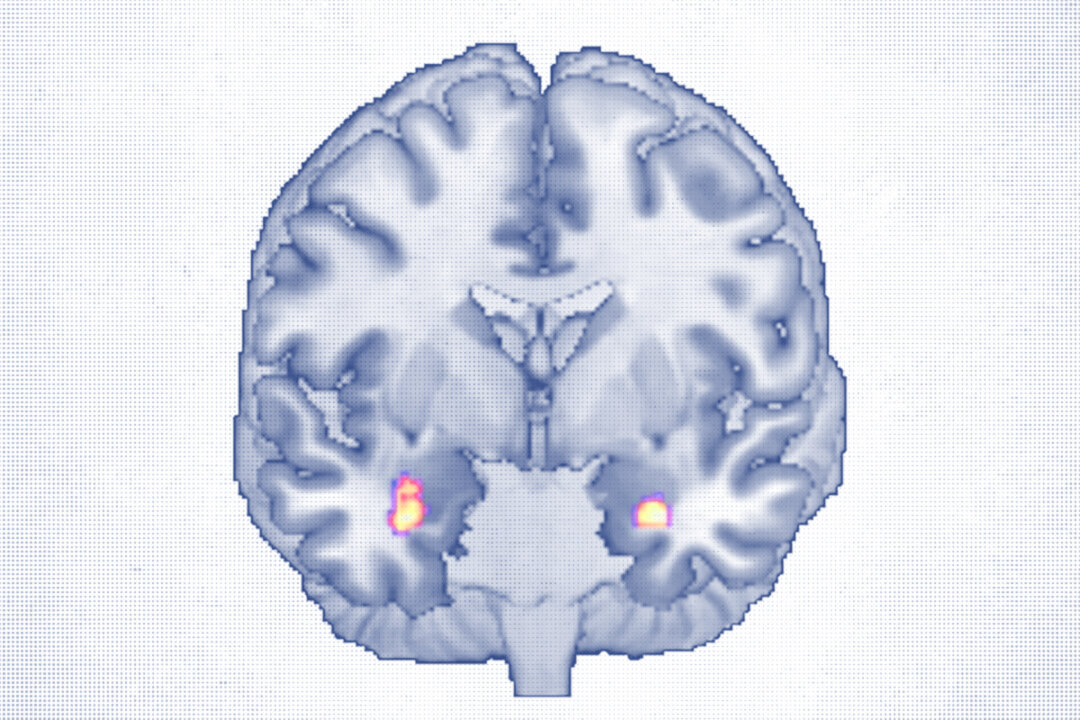
A brain imaging study published in Translational Psychiatry found that adults who completed a course of cognitive behavioral therapy (CBT) showed measurable growth in regions of the brain responsible for emotion processing and mood regulation. These areas, often weakened in chronic depression, appeared to strengthen over the course of treatment.
“For the first time, we have a reliable biomarker for the effect of psychotherapy on brain structure,” senior researcher Ronny Redlich, head of biological and clinical psychology at Martin Luther University Halle-Wittenberg in Germany, said in a statement.
What the Brain Scans Showed
“There is a clear connection between the brain and the mind, including between mental disorders and our brain,” Redlich told The Epoch Times in an email.
The idea that the brain can adapt and change is based on the concept of neuroplasticity.
The study followed 30 adults, ages 18 to 65, with major depressive disorder who received about 20 CBT sessions over 40 weeks. High-resolution MRI scans before and after treatment revealed increased gray matter volume in the amygdala, a key region for emotional processing, and the anterior hippocampus, which is involved in memory and mood regulation.
Both areas are known to shrink in people with depression, so growth here may signal recovery, the researchers noted.
By the end of the study, 19 of the 30 participants no longer met the clinical diagnosis for depression.
Increased gray matter in the amygdala was correlated with a greater ability to perceive emotions, particularly one’s own, Redlich said.
That ability, known as emotional awareness, is often impaired in those with depression. Many people with a condition called alexithymia—a difficulty identifying or expressing emotions—find it harder to process what they feel. CBT, long known to help people manage depression, is designed to improve this skill.
“Psychotherapy works and psychotherapy changes the brain,” Redlich said. “Mental disorders are not a personal weakness. They’re linked to physical changes in the brain. Psychotherapy can help ‘repair’ those connections.”
About one-third of the participants were taking antidepressants, so it’s possible that some of the brain changes were related to medication. However, even after accounting for that, the link between brain changes and therapy remained significant.
Additionally, the study did not include an untreated depression group, so it’s possible that some brain changes could have happened naturally. Still, the researchers believe that the results support the idea that developing emotional skills through talk therapy—such as CBT—can shape the brain.
How CBT Might Reshape the Brain
CBT is one of the most widely recommended and rigorously studied therapies for depression. It focuses on breaking cycles of negative thinking and teaching practical skills for managing stress, emotions, and daily challenges.
This kind of targeted mental “training” changes people’s thinking, slowly changing how the brain functions.
Every major health organization recognizes CBT, or its variants, as the only evidence-based psychotherapy proven effective across conditions, Mike Abrams, a clinical psychologist and author of several textbooks on cognitive therapy, told The Epoch Times.
Part of its effectiveness, Abrams said, comes from people developing emotional awareness and practicing a kind of flexibility that fosters acceptance and resilience.
“All the CBTs inherently have [a] stoic philosophy, which is a lifestyle of acceptance,” he said.
Essentially, everything that one feels, to some extent, is a function of what they’re thinking. Instead of fighting every uncomfortable emotion or thought, CBT encourages people to acknowledge them, reflect, and respond more intentionally.
“A good CBT therapist, if they’re really doing their job, [is] listening for things that people say that are not rational and guiding the person to see that their own demanding thinking, their own rigidity, is leading to their disturbance,” Abrams said.
Over time, this training may strengthen the brain’s circuits involved in self-regulation, emotional insight, and resilience, providing a possible explanation for the structural changes seen in the study.
“Ultimately, changes in thinking and behavior always lead to changes in the brain, even in healthy individuals, and that is good news,” Redlich said. “We can decide for ourselves, at least to some extent, how we connect our brains and what we teach them, also mentally.”
Looking Ahead
Redlich and his team plan to follow study participants for several years to determine whether these brain changes last, and whether they predict who will stay well or relapse. Eventually, the researchers hope that brain imaging, possibly combined with artificial intelligence, could help personalize treatment decisions.
For now, the study shows that what one thinks can shape the brain. And for some people with depression, that means healing may not start with a pill—it might begin with a thought.