Cardiac arrest, also known as asystole and sudden cardiac arrest, refers to the sudden loss of function and the stopping of the heart. The patient may or may not have been diagnosed with heart disease prior to cardiac arrest. Cardiac arrest may occur suddenly or follow other symptoms; patients can easily die if proper first aid measures are not taken. This article will guide you through the causes, symptoms, first aid, and treatment of cardiac arrest, with illustrations.
Cardiac Arrest Versus Heart Attack
You may be wondering: Is cardiac arrest the same as a heart attack (myocardial infarction)? Actually, they are two different conditions.
A heart attack is caused by the blockage of blood vessels (coronary arteries) that supply nutrients to the heart, resulting in myocardial ischemia and necrosis; thus, a heart attack can indeed cause cardiac arrest. However, the main cause of cardiac arrest is actually related to the electrical system that controls the heart’s rhythm.
What Are the Causes of Cardiac Arrest?
The beating of the heart occurs when an electric current is sent through the sinoatrial node, which transmits the signal to the myocardium through the conduction pathway, thereby stimulating the contraction of the myocardium. When the electrical conduction system malfunctions, it results in cardiac arrhythmia, which is the leading cause of cardiac arrest.
There are many types of arrhythmias, including ventricular tachycardia, atrial fibrillation, ventricular fibrillation, and bradycardia. The most common cause of cardiac arrest is ventricular fibrillation, which occurs when the heart’s chambers beat suddenly and chaotically, preventing blood from being pumped smoothly.
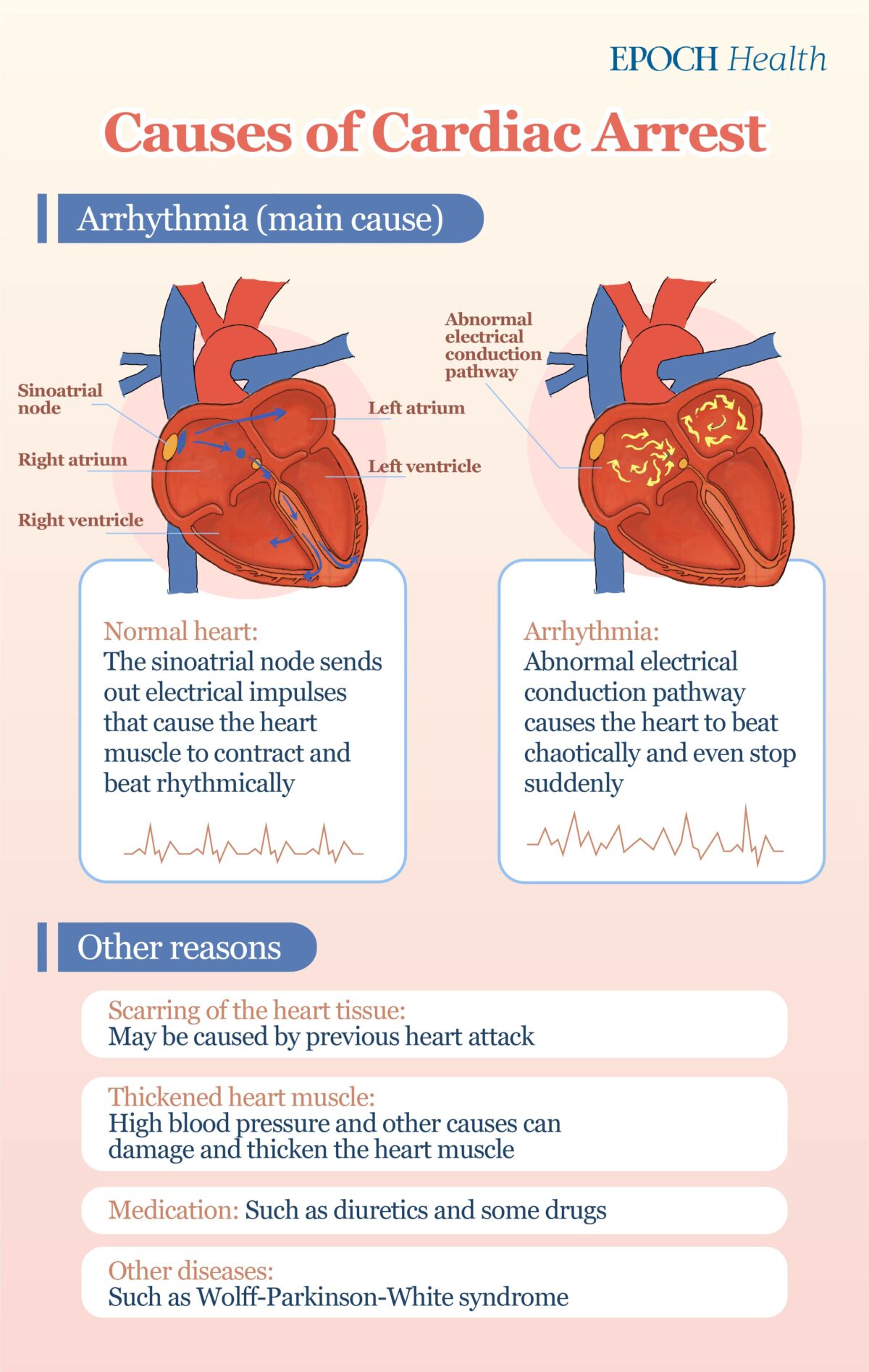
Scarring of the Heart Tissue
This may be caused by previous coronary heart disease (such as heart attack) or other reasons. These scars can interfere with the heart’s electrical system, causing life-threatening ventricular arrhythmias.
Thickened Heart Muscle (Cardiomyopathy)
High blood pressure, heart valve disease, or other problems can damage and thicken the heart muscle, making the patient more prone to irregular heartbeats, heart failure, and cardiac arrest.
Medication
An imbalance of potassium and magnesium in the blood caused by the use of diuretics may also lead to arrhythmia and cardiac arrest. Oddly, drugs that treat arrhythmias can sometimes cause ventricular arrhythmias, and this is called a proarrhythmic effect. The abuse of certain drugs can also lead to cardiac arrest.
Other Diseases
Some conditions that predispose a person to abnormalities in the electrical flow of the heart, such as Wolff-Parkinson-White syndrome and Long QT syndrome, may increase the risk of cardiac arrest in children and young adults.
3 Main Symptoms of Cardiac Arrest
There may be some warning signs before a cardiac arrest, such as tightness in the chest, difficulty breathing, palpitations, and weakness. However, most cardiac arrests occur with little warning.
So what are the symptoms of cardiac arrest?
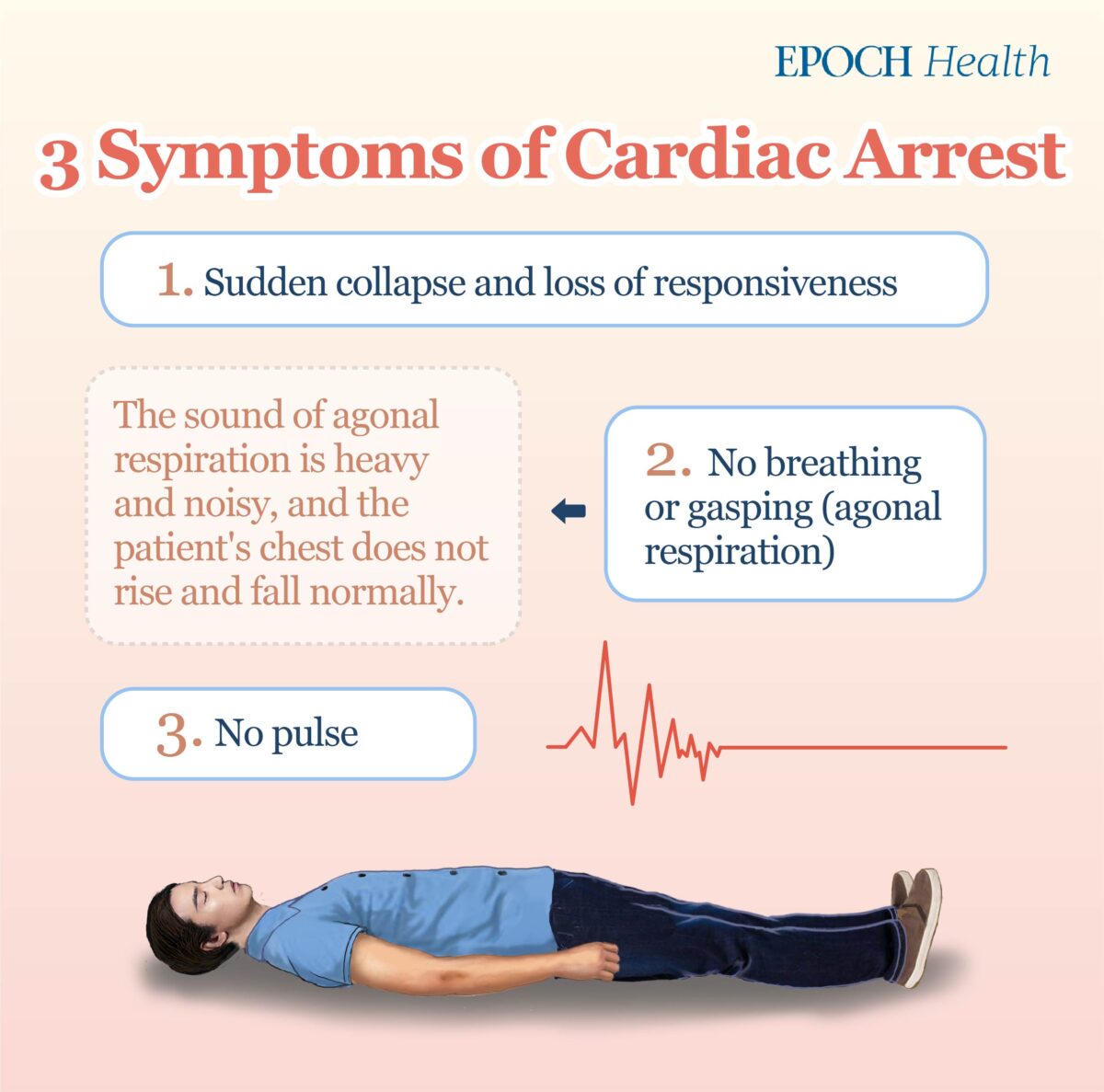
- Sudden collapse and loss of responsiveness
- No breathing or gasping (agonal respiration). Gasping usually has an interval of more than seven seconds between each breath; the sound is heavy and noisy, and the chest does not rise and fall like normal breathing.
- No pulse
2 First Aid Methods for Cardiac Arrest
If the heartbeat is not restored quickly after cardiac arrest, it will lead to hypoxia of organs and tissues throughout the body, resulting in damage and necrosis, and even death. Therefore, first aid must be administered to the patient as soon as possible.
It is possible to save the patient if first aid is administered within a few minutes.
When encountering a person in cardiac arrest, we should first calm down and confirm that the surrounding environment is safe. For example, if the patient collapses on the road, we should first move him/her to a safer place to avoid getting hit by a vehicle.
Then, follow the steps below to provide first aid to a patient in cardiac arrest.
- Step 1: Speak to the patient and tap him/her on the shoulder to check for a response.
- Step 2: Ask someone nearby to call an ambulance immediately, and ask another person to get an AED (automated external defibrillator).
- Step 3: Check the patient’s breathing, either by looking for air in and out of the mouth and nose, or by looking for a rise and fall in the chest. The time from confirming the patient’s unresponsiveness to checking for breathing should not exceed 10 seconds. Usually, the interval between each breath is about seven seconds; therefore, CPR (cardiopulmonary resuscitation) should be administered immediately after confirming that the patient has not breathed for more than seven seconds or is showing agonal respiration.
- Step 4: As it arrives at the scene, turn on the AED and follow the voice prompts. CPR and AED should be performed alternately until the patient regains heartbeat, is breathing or awake, or until professional paramedics arrive at the scene.
1. How to Do CPR
Follow these steps to administer CPR to a patient:
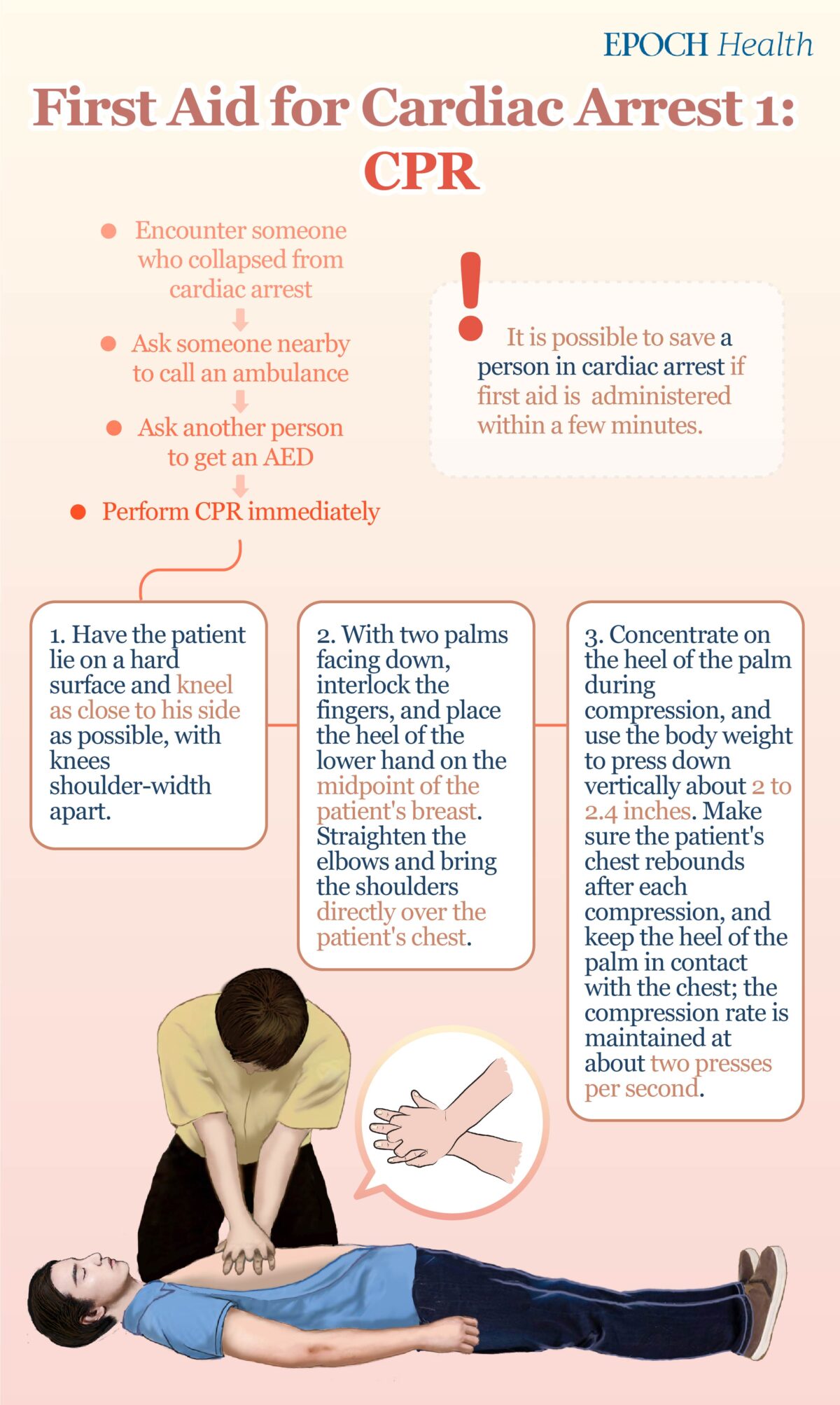
- First, make sure that the patient is lying on a hard surface; remove the patient’s clothing so that the AED pad can be quickly attached when the AED arrives. The person performing CPR should kneel by the patient’s side with the knees shoulder-width apart, and stay as close to the patient as possible.
- With two palms facing the same side, interlock the fingers of one hand on top of the other, and place the heel of the lower hand on the midpoint of the patient’s breast. Straighten the elbows and bring the shoulders directly over the patient’s chest.
- Concentrate on the heel of the palm during compression, and use the body weight to press down vertically about 2 to 2.4 inches (5–6 centimeters). Make sure the patient’s chest rebounds after each compression, and keep the heel of the palm in contact with the patient’s chest; the compression rate is maintained at about two presses per second.
If other people on the scene know how to perform CPR, they can take turns when the first person is exhausted. There should be as little inactivity time as possible between rotations—ideally no inactivity time at all.
2. How to Use an AED
When an AED is available, the assistance of another person is required. He/she should follow the “turn on, attach, plug, and shock” steps to use it. During AED setup, the rescuer must not stop performing CPR until the AED voice instructs not to touch the patient.
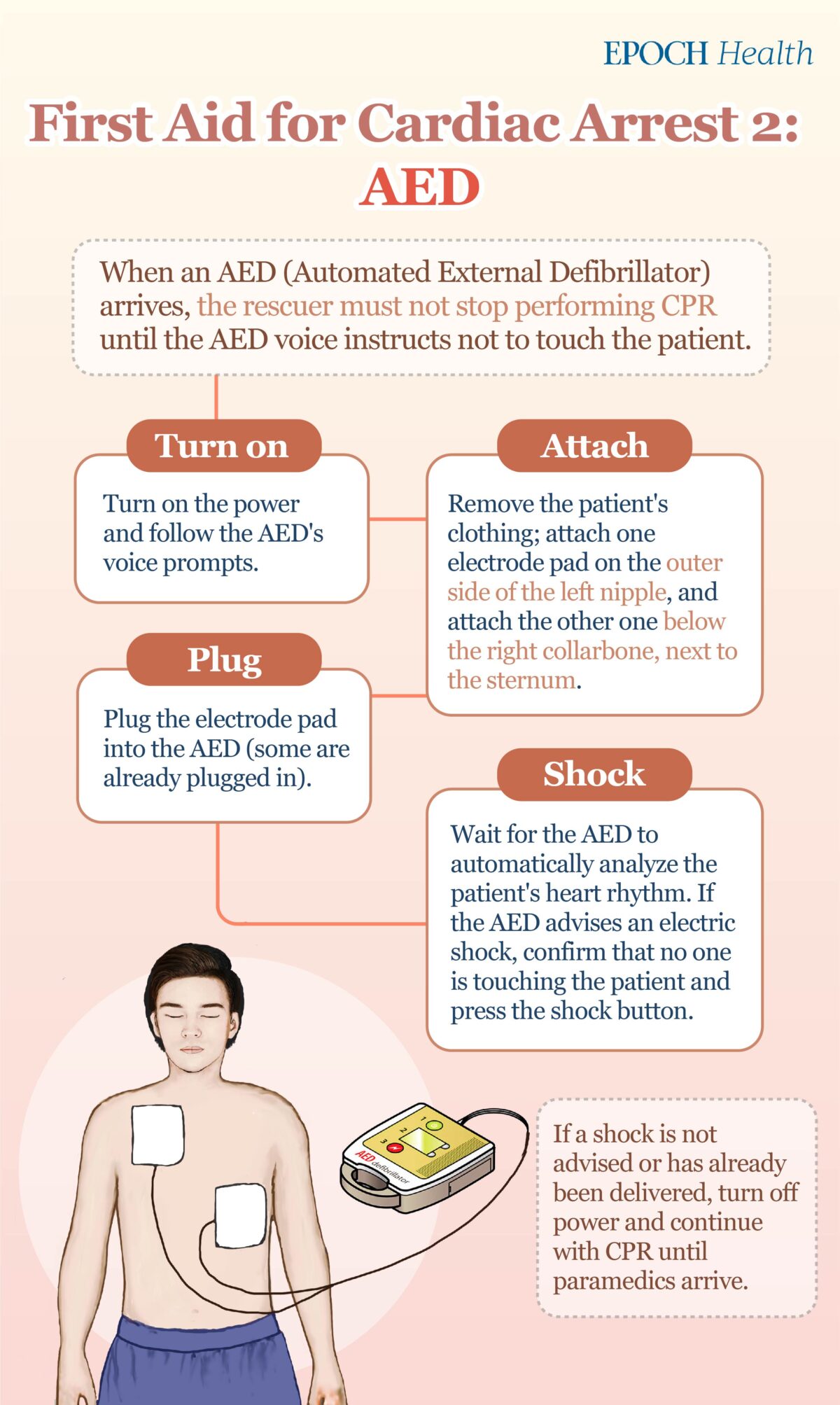
- Turn on: Open the AED box, turn on the power, and follow the AED’s voice prompts.
- Attach: Remove the patient’s clothing; attach one electrode pad on the outer side of the left nipple, and attach the other one below the right collarbone, next to the sternum. For patients over 8 years old or 55 pounds (25 kilograms) in weight, an adult pad should be used; for patients below the standard, a pediatric pad should be used (an adult pad can be used if a pediatric pad is not available).
- Plug: Plug the electrode pad into the AED. Some AEDs already have the electrode pad plugged in.
- Shock: The AED will automatically analyze the patient’s heart rhythm and instruct not to touch the patient. If a defibrillation shock is required after analysis, please first yell “CLEAR!”; after confirming that no one is touching the patient, press the shock button to deliver an electric shock. If a defibrillation shock is not advised or has already been delivered, turn off the power and continue with CPR until paramedics arrive.
There are a few things to keep in mind when using an AED:
If the pad cannot attach to the skin due to excessive chest hair on the patient, tear off the pad with force to remove the chest hair and replace it with a new pad. If the AED comes with a razor, it can also be used to shave chest hair. If there is a transdermal patch on the patient, remove it and wipe off the drug residue on the skin before attaching the shock pad. If the patient has a pacemaker (there may be a round or square bump on the body), avoid placing the shock pad directly on the bump.
Patients who survive cardiac arrest need to be examined by a doctor to understand the cause of the cardiac arrest and receive corresponding treatment to reduce the chance of recurrence.