The very trait that makes your metabolism healthy can make cancer deadly.
Metabolic flexibility—the cells’ ability to switch efficiently between fuel sources such as glucose and fat—is usually a hallmark of good health. However, when cancer cells gain the same adaptability, it becomes their survival advantage, enabling tumors to evade treatment and resist even the most targeted therapies.
This paradox is forcing researchers to rethink decades of cancer treatment strategies and develop new approaches that simultaneously attack tumors on multiple metabolic fronts.
Cancer’s Multiple Fuel Sources
For nearly a century, our understanding of cancer metabolism was shaped by German biochemist Otto Warburg, who observed that cancer cells consume large amounts of glucose even when oxygen is abundant. The “Warburg effect” led scientists to believe that tumors relied almost exclusively on sugar for fuel, inspiring metabolic therapies aimed at starving cancer by cutting off its glucose supply.
However, Warburg’s model no longer reflects the full story.
“When a treatment blocks one fuel line, like a drug that targets glucose, the cancer cells simply switch to glutamine or fats to stay alive,” Michael Enwere, a cancer scientist and integrative oncology researcher specializing in metabolic interventions, told The Epoch Times. “It’s like a survivalist who, when you cut off their food supply, starts efficiently hunting and foraging to avoid starvation.”
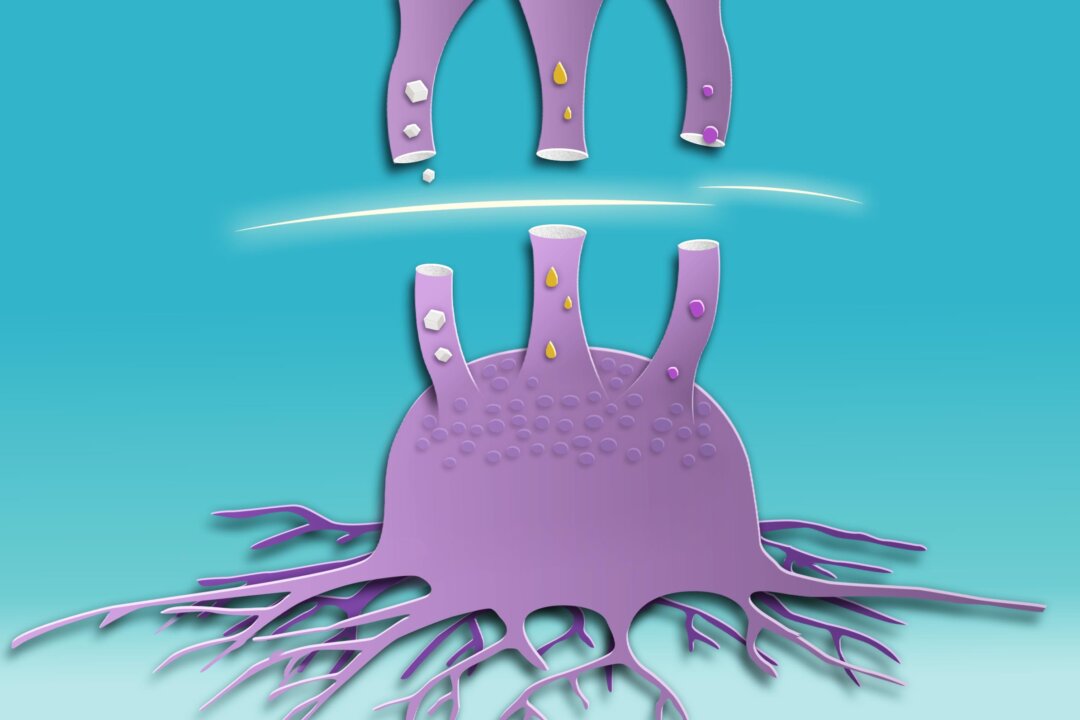
Newer research shows that many cancers are far more adaptable than once thought. Instead of relying on a single energy source, malignant tumors exploit whatever fuel is available to sustain their growth. When glucose is scarce, they may increase glutamine (an essential amino acid) metabolism or tap into fatty acids. Some even metabolize ketones, the fuel the body produces during fasting or ketogenic diets. This metabolic flexibility helps explain why interventions such as strict carbohydrate restriction or ketogenic diets sometimes show early promise but don’t necessarily produce lasting results.
A study published in the Journal of Experimental & Clinical Cancer Research found that glutamine metabolism helps cancer grow and evade the immune system. While drugs can block the pathway, cancer often finds alternatives.
The Metabolic Survivalists
Aggressive cancers such as glioblastoma and triple-negative breast cancer are the ultimate metabolic survivalists, Enwere said.
Conventional therapies that are designed to target a specific pathway often fail with these types of cancer because they are playing “Whac-A-Mole” with a dynamic, adaptable metabolic network, he added.
“When I was at the National Cancer Institute, I worked in a department called Drug Resistance,” Mona Jhaveri, who has a doctorate in biochemistry and molecular biology, told The Epoch Times. “The entire field was dedicated to understanding why cells become resistant to chemotherapy and other therapies.”
The complexity of cancer’s metabolic behavior is striking. “ You can take cells from one tumor, and you will find various versions of these cells operating differently. That’s another reason why cancer is so tricky, because they are not all one kind,” Jhaveri said.
Therefore, any single treatment approach is ineffective. “We all have cancer cells in our bodies. It’s our immune system that keeps them at bay. We need a war chest of tools—it can’t just be the same chemo and the same regimen,” she added.
The Future of Cancer Treatment
Scientists are now developing approaches that target many fuel pathways simultaneously.
Instead of cutting off just glucose, for example, some therapies inhibit both glucose and glutamine metabolism—the two primary fuels many tumors rely on. Limiting cancer cells’ ability to switch between nutrients can increase their vulnerability to treatment.
Cancer treatment needs to be multifaceted, addressing not only genetic mutations but also the underlying metabolic function that sustains tumors. A systematic review published in Onco, led by Enwere, found that metabolic-targeted therapies, including natural compounds such as curcumin, berberine, and high-dose vitamins C and D3, show promise in disrupting cancer’s energy pathways and overcoming resistance to conventional treatments. Combining these approaches with chemotherapy, radiation, and immunotherapy offers a personalized and low-toxicity approach for patients with hard-to-treat tumors.
“All four show promise, but intravenous high-dose vitamin C (IVC) and berberine currently stand out,” Enwere said.
“IVC has the clearest translational footprint today [and] berberine is the most promising for glutamine-driven tumors once delivery issues are solved,” he said. It is currently not absorbed well by the body and has gastrointestinal side effects.
In the next decade, Enwere envisions a shift from a solely genetic view of cancer to one that integrates multiple layers of data, including metabolism. He foresees using metabolic interventions to sensitize tumors. For example, a short ketogenic diet combined with a glutamine-blocking drug to “prime” tumors for a better response to chemotherapy or immunotherapy. He added that metabolic-targeted therapies are nearing having a place in standard care.
“We are at a pivotal translational tipping point. The preclinical evidence is robust and compelling, and we are now seeing a growing number of promising phase 2 clinical trials, such as one with high-dose IV [intravenous] vitamin C in rectal cancer,” he said.
1 Patient’s Metabolic Experiment
When Pete Sulack, a chiropractor, was diagnosed with terminal brain cancer in late 2024, doctors gave him only months to live. Instead of relying solely on conventional treatment, he adopted a metabolic protocol focused on three key principles:
- Limiting glucose availability to cancer cells
- Supporting mitochondrial function
- Enhancing oxygenation and detoxification
As part of this approach, he followed a therapeutic ketogenic diet, which stabilized his blood sugar and reduced insulin levels. “The goal wasn’t just to starve cancer, but to strengthen healthy cells,” he told The Epoch Times. He focused on understanding how his cells’ energy use influenced both health and disease.
In March, doctors declared Sulack in full remission.
While his approach is personalized and anecdotal, it illustrates a broader concept: Metabolic interventions may influence cancer’s ability to adapt and survive.
Building Your Metabolic Flexibility
While you can’t control cancer’s metabolism, you can take a page from its book by strengthening your own metabolic flexibility—a state that keeps healthy cells adaptable and resistant to dysfunction that can lead to cancer.
Metabolic flexibility isn’t just about burning fat or glucose—it’s about how well your mitochondria can shift gears as conditions change. Often called the powerhouses of the cell, the mitochondria are responsible for converting different fuels into energy, allowing your body to switch between burning fat or glucose as needed. Even small daily habits can cumulatively strengthen adaptability over time. When mitochondria are strong, your body is better equipped to handle metabolic challenges such as illness.
Regular exercise is one of the most effective ways to enhance this adaptability. Both aerobic training and resistance work stimulate the creation of new, more efficient mitochondria, improving how cells use and store energy. Even simple habits, such as taking brisk walks after meals or engaging in brief bursts of higher-intensity movement, can help.
Diet diversity also plays a key role. Constantly eating the same macronutrient balance can make metabolism rigid, whereas cycling between carbohydrate-rich and fat-based fuel periods—through time-restricted eating, low-carb days, or occasional fasting—encourages cells to remain metabolically flexible. For most people, there’s no need for extreme diets. It’s about training your metabolism to handle both abundance and scarcity.
Food quality also matters. “Poor nutrition may play a role in creating tumor-friendly environments—pushing cells into stress and making them more likely to become malignant,” Jhaveri said. Persistently high blood sugar and chronic inflammation from ultra-processed foods and refined sugar can damage mitochondria and promote the same metabolic inflexibility in which cancer thrives.
“With so many processed foods, we’re likely creating what we call tumor microenvironments,” she said. “Obesity is also linked to cancer—it promotes inflammation and the release of cytokines that create pro-tumor conditions.”
The Role of Human Connection in Metabolic Health
Metabolic health isn’t just about food and exercise. Jhaveri referenced a 2016 study published in Social Cognitive and Affective Neuroscience, which showed that when dogs were given a choice between food and praise, brain activity in their reward centers was often equal to or greater in response to praise. She believes social interaction and positive reinforcement optimize the body’s internal environment to foster healthy cells.
While that may seem far from metabolism, social connection influences hormones, inflammation, and even mitochondrial signaling.
Just as our cells need flexibility to thrive, our bodies also rely on human connection to stay resilient, a reminder that health operates on both molecular and social levels. “There are unspoken molecular interactions that happen when we come together. When humans come together, it helps them in survival,” Jhaveri said.
Building metabolic flexibility through movement, nourishment, and connection essentially future-proofs your cells, making them less vulnerable to the metabolic chaos cancer cells exploit.
“I’m living proof that when you change the metabolic environment of the body, by removing the fuel cancer thrives on and restoring what supports health, healing becomes possible,” Sulack said.
You can’t control cancer’s metabolism, but you can optimize your own.