Breast cancer accounts for roughly 30 percent of all new cancer diagnoses in women each year, making it the most common cancer among women in the United States after skin cancers. The lifetime risk for a woman developing breast cancer is about 1 in 8.
Breast cancer incidence has been increasing in recent years, with a slightly higher rate in women under 50. On a more hopeful note, about two-thirds of cases are identified at an early stage, when the cancer hasn’t spread beyond the breast, and treatment is generally more effective.
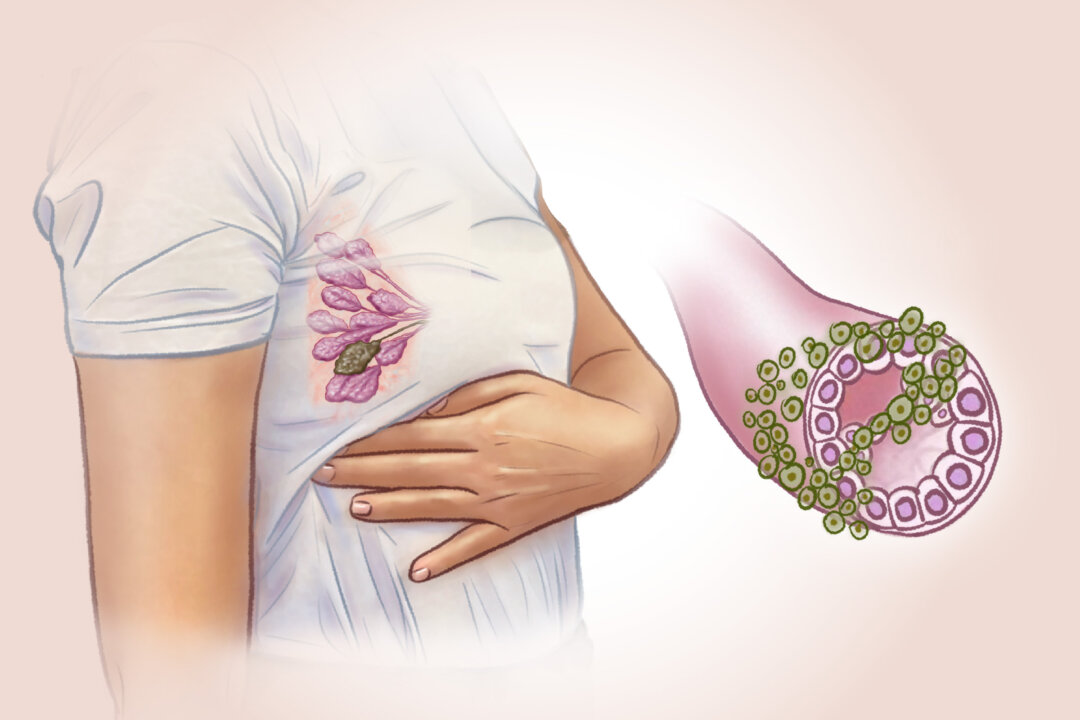
[epoch_component type=”photo_gallery” position=”center” section_title=”(Illustration by The Epoch Times, Shutterstock)” width=”900″ items=”5924409,” image_stays=”false” stays_for_paragraphs=””][/epoch_component]
[shortcut_anchor id=”anchor_1759527697534″ label=”Types”]What Are the Types of Breast Cancer?[/shortcut_anchor]
Most breast cancers are carcinomas, which begin in the epithelial cells—the body’s protective lining cells that cover surfaces and organs.
The most common type of breast cancer is invasive ductal carcinoma, which makes up 70 percent to 80 percent of all cases. This cancer starts in the milk ducts, the tubes that transport milk. Invasive lobular carcinoma begins in the milk-producing glands and accounts for 10 percent to 15 percent of cases. This cancer often doesn’t form a distinct lump, making it harder to detect on mammograms.
There are also early-stage forms called ductal carcinoma in situ and lobular carcinoma in situ. These conditions refer to abnormal cells that may progress to invasive cancer or indicate a higher future breast cancer risk.
[shortcut_anchor id=”anchor_1759527703543″ label=”Symptoms”]What Are the Symptoms and Early Signs of Breast Cancer?[/shortcut_anchor]
Breast cancer often causes no pain in its early stages and may not show obvious symptoms.
Warning Signs
Having these symptoms doesn’t always mean breast cancer, but it’s important to see a doctor if any of the following changes appear:
- A new lump in the breast or armpit (as many as 90 percent of breast lumps are benign, meaning noncancerous)
- Thickening or swelling in part of the breast
- Skin irritation or dimpling on the breast
- Redness or flaky skin on the breast
- Nipple retraction or pain in the nipple area
- Nipple discharge that is not breast milk, which may include blood
- Changes in the nipple’s position or orientation
- Noticeable changes in breast size or shape
- Pain in any part of the breast
- A sore or ulcer on the breast or nipple, which may spread to the areola
Advanced Cancer Symptoms
When breast cancer spreads beyond the breast, it may cause additional symptoms, such as:
- Bone pain
- Shortness of breath
- Swollen lymph nodes in the armpit near the affected breast
- Unexplained weight loss
- Difficulty sleeping
- Feeling unwell without a clear reason
Common Symptoms in Men
Breast cancer can also occur in men, accounting for less than 1 percent of all diagnosed cases.
- A lump or swelling in the chest or armpit
- Nipple discharge, possibly with blood
- Changes in chest size or shape
- Sores or ulcers on the chest
- Changes in the nipple’s appearance, such as an inverted nipple or a rash resembling eczema
[shortcut_anchor id=”anchor_1759527712399″ label=”Causes”]What Causes Breast Cancer?[/shortcut_anchor]
Breast cancer, like many other cancers, develops when genetic changes, or mutations, occur in critical genes that regulate cell growth, division, or DNA repair. These mutations allow cells to grow uncontrollably, eventually forming a tumor.
Several factors can increase your risk.
Uncontrollable Risk Factors
Age is the strongest risk factor for breast cancer, as about 80 percent of cases occur in women over the age of 50, while the disease is rare in women under 30. About half of breast cancers occur in women with no known risk factors other than getting older.
Other uncontrollable risk factors include:
- Family History: Having a first-degree relative with breast cancer doubles or triples a woman’s risk. A family history of ovarian cancer or breast cancer in a male relative also increases risk.
- Genes: Inherited gene mutations such as BRCA1 and BRCA2 account for 5 percent to 10 percent of all cases, but may cause up to 25 percent of cases in women under 30.
- Previous Breast Conditions: A history of breast cancer or certain benign breast conditions increases risk.
- Dense Breast Tissue: Breasts with more glandular and connective tissue and less fatty tissue carry a higher risk.
- Liver Diseases: A 2024 study found that FGF21, a liver-secreted protein, is linked to several cancers, including breast cancer, especially in people with conditions such as fatty liver disease.
- Ethnicity: Black women have higher death rates, while Caucasian, Asian, and Pacific Islander women are more often diagnosed at earlier stages.
- Height: Taller women have a higher risk, possibly due to early growth factors such as nutrition, hormones, or genetics.
Lifestyle Factors
Certain lifestyle choices can also increase breast cancer risk:
- Obesity: Being overweight or obese, especially after menopause, increases risk due to higher hormone and insulin levels.
- Alcohol Use: Drinking alcohol raises risk, with heavier use linked to greater risk.
- Endocrine-Disrupting Chemicals: Substances in plastics, cookware, pesticides, and personal care products can interfere with hormone function, often blocking estrogen receptors and raising estrogen levels.
- Physical Inactivity: Inactivity increases risk, especially in post-menopausal women. Regular activity may lower breast cancer risk by helping to manage body weight, inflammation, and hormone levels.
- Night Shift Work: Women who work night shifts, such as nurses, may have an increased risk of breast cancer. This could be linked to changes in melatonin levels caused by nighttime light exposure.
- Stress: Traumatic events and chronic stress may weaken the immune system and raise cortisol levels (stress hormones), potentially increasing cancer risk.
Certain medical interventions may also affect risk:
- Antipsychotic Drugs: Use of antipsychotic medications may raise the risk of breast cancer by about 30 percent.
- Hormonal IUDs: A 2024 study found that women aged 15 to 49 who use hormonal intrauterine devices (a small contraceptive device placed inside the uterus) have a 40 percent higher risk of developing breast cancer compared to those who do not use them.
- Exposure to Diethylstilbestrol (DES): Women who took this drug during pregnancy between 1940 and 1971 have a higher risk of breast cancer. Their daughters, who were exposed to DES in the womb, may also face an increased risk.
- Radiation Therapy: Women who received chest radiation therapy during their teens or young adulthood—when breasts are still developing—face a significantly higher risk. Radiation after age 40 to 45 does not appear to increase risk.
Risk Factors in Men
Although breast cancer is much less common in men, certain factors can increase their risk of developing the disease.
- Estrogen Receptor Positive (ER+): Most male breast cancers are ER+, meaning they grow in response to the hormone estrogen.
- Gene Mutations: Men with breast cancer are more likely to carry genetic mutations such as BRCA that increase their risk.
[shortcut_anchor id=”anchor_1759527726511″ label=”Diagnosis”]How Is Breast Cancer Diagnosed?[/shortcut_anchor]
Detecting breast cancer early is critical for effective treatment. Pay attention to unusual changes in your breast, like a lump, pain, or change in size. Screening and diagnostic methods such as mammograms, ultrasounds, MRIs, and biopsies can help find breast cancer in its earliest stages.
1. Screening
Several screening tests are available, including:
- Mammogram: The most effective tool for early breast cancer detection is a mammogram, a specialized breast X-ray. The U.S. Preventive Services Task Force recommends mammograms every two years for women ages 40 to 74 at average risk. Mammograms also carry certain risks, such as false positives and unnecessary biopsies. Many women choose to delay screening if they are considered at lower risk for breast cancer.
- Breast MRI: Uses magnets and radio waves to create detailed breast images. It is typically used alongside mammograms for women at high risk of breast cancer. Due to higher false positive rates, it is not recommended for women at average risk.
- Clinical Breast Exam: A physical exam performed by a doctor or nurse to check for lumps or changes in the breast by touch.
- Breast Self-Awareness: Familiarity with the normal look and feel of the breasts helps people notice unusual changes such as lumps, pain, or size differences.
2. Diagnosis
If a screening mammogram shows abnormal results, doctors perform additional tests to determine whether breast cancer is present:
- Breast Ultrasound: Uses sound waves to create images (sonograms) of breast tissue.
- Diagnostic Mammogram: A more detailed and targeted breast X-ray than a screening mammogram.
- Biopsy: Involves removing breast tissue or fluid for microscopic examination to diagnose cancer.
- Molecular Breast Imaging: Involves injecting a radioactive tracer into the arm, which travels to breast tissue. A special camera then captures images of the tracer within the breast.
3. Additional Tests
If breast cancer is diagnosed, further tests help guide treatment. For example:
- Hormone receptor tests show whether the cancer grows in response to estrogen or progesterone.
- HER2 testing measures protein levels that affect how fast the cancer grows.
- Genetic testing checks for inherited mutations such as BRCA that may influence treatment decisions.
[shortcut_anchor id=”anchor_1759527745465″ label=”Stages”]What Are the Stages of Breast Cancer?[/shortcut_anchor]
Staging is the process of determining how far breast cancer has spread. It helps guide treatment decisions and is based on factors such as tumor size, lymph node involvement, metastasis, and hormone receptor status.
There are five stages of breast cancer:
- Stage 0: Cancer is in its earliest form and has not spread beyond where it started (called “in situ”).
- Stage 1: Cancer has begun to spread into nearby breast tissue or lymph nodes. A tumor may be present, or small groups of cancer cells may be found.
- Stage 2: The tumor is larger (between 2 and 5 centimeters), and/or cancer has spread to a few nearby lymph nodes.
- Stage 3: Cancer is more advanced. It may have grown into the chest wall or skin, and/or spread to several lymph nodes.
- Stage 4: Cancer has spread beyond the breast and nearby lymph nodes to other parts of the body, such as the bones, liver, or lungs. This is known as metastatic breast cancer.
[shortcut_anchor id=”anchor_1759527751417″ label=”Treatments”]What Are the Treatments for Breast Cancer?[/shortcut_anchor]
Breast cancer treatment depends on the stage and type of cancer. Treatments for men are similar to those for women.
1. Surgery
Breast cancer is mainly treated with surgery, often alongside chemotherapy, radiation therapy, or both. The main surgical options are:
- Lumpectomy: Removes the tumor and a small amount of surrounding tissue. It’s usually used for early-stage breast cancer with small tumors.
- Mastectomy: Removes the entire breast. Some types may preserve the skin or nipple area, and breast reconstruction can often be done at the same time. In certain high-risk cases, such as those involving BRCA mutations, both breasts may be removed (double mastectomy) to reduce future cancer risk.
2. Chemotherapy
Chemotherapy uses strong drugs administered orally or through an IV to kill cancer cells or slow their growth. It may be given before surgery to shrink tumors.
3. Radiation Therapy
Radiation therapy uses high-energy beams to kill breast cancer cells. It may be used before surgery to shrink tumors or after surgery to destroy any leftover cancer cells. Doctors can deliver radiation from outside the body with machines that shape and aim the beams precisely, or from inside the body by placing tiny radioactive seeds near the tumor.
The goal is always to destroy the cancer cells while protecting as much healthy tissue as possible.
4. Proton Therapy
Proton therapy is a type of radiation treatment that uses protons—positively charged particles—to destroy breast cancer cells by damaging their DNA. It is a more precise form of radiation therapy compared with traditional photon radiation. While photon beams continue past the target and can damage nearby organs such as the heart and lungs, proton beams stop after reaching the tumor, sparing surrounding healthy tissues.
5. Targeted Therapy
Targeted therapy works by interfering with specific molecules or genes that cancer cells rely on to survive, grow, and spread. These treatments use drugs or substances designed to identify and attack cancer cells precisely while limiting damage to healthy cells.
To determine which targeted therapies may work best, doctors often perform biomarker tests to see how the cancer will respond to certain drugs.
Several medications are available that work in different ways—some are engineered proteins that stick to cancer cells and destroy them, while others block the signals that tell cancer cells to grow or prevent them from repairing themselves when damaged.
6. Hormone Therapy
Also known as endocrine therapy, hormone therapy treats hormone-sensitive breast cancer by either blocking hormone production or preventing hormones from affecting cancer cells, thereby slowing or stopping tumor growth.
7. Immunotherapy
Immunotherapy boosts the body’s immune system to fight cancer. In breast cancer, immune checkpoint inhibitors work by blocking proteins that stop immune cells (T cells) from attacking cancer. This helps the immune system recognize and destroy cancer cells more effectively.
8. Intravenous Vitamin C
Some research suggests that vitamin C may be a valuable supportive therapy in breast cancer treatment. A 2020 review found that high-dose intravenous vitamin C provided anti-inflammatory and anticancer effects without interfering with certain treatments and some chemotherapy drugs.
9. Acupuncture
Acupuncture may alleviate insomnia, hot flashes, fatigue, anxiety, treatment-related joint pain, and other symptoms in breast cancer survivors.
[shortcut_anchor id=”anchor_1759527762057″ label=”Lifestyle Approaches”]What Are the Natural and Lifestyle Approaches to Breast Cancer?[/shortcut_anchor]
Some people use natural or lifestyle approaches to support recovery and improve quality of life. These methods are best used alongside medical treatment.
1. Antioxidant-Filled Diet
Many of the same foods that promote overall health also help lower inflammation and provide nutrients with potential anticancer properties.
A key benefit of a healthy diet is its high content of antioxidants—compounds found in plant-based foods that protect cells by neutralizing free radicals, which can damage DNA and contribute to cancer development. Examples include:
- Vitamin C: Citrus fruits and red and green peppers
- Vitamin E: Almonds and hazelnuts
- Polyphenols: Broccoli, olive oil, and oats
- Carotenoids: Spinach, carrots, and mangoes
It’s also important to limit certain foods and beverages during treatment and recovery. Processed and high-sugar foods may contribute to inflammation and weight gain. Trans fats and high fat diet may increase breast cancer mortality. Alcohol should be avoided completely during treatment, as any amount may increase cancer risk.
2. Supplements
Some nutritional supplements may help with breast cancer recovery:
- Vitamin D: Low vitamin D levels have been linked to higher breast cancer risk. Some breast cancer treatments can lead to bone loss, which vitamin D supplementation may help prevent by supporting bone health.
- Omega-3 Fatty Acids: A 2024 preclinical study in mice found that omega-3 fatty acids, known for their anti-inflammatory properties, may affect how the body responds to chemotherapy. More research is needed to understand whether these findings apply to people with breast cancer.
3. Self-Massaging Acupoints
Self-massage of certain acupuncture points may help reduce stress and support well-being.
Chen Bo Sheng, a traditional Chinese medicine practitioner focused on integrative cancer care, recommends self-massaging the following acupuncture points:
- Inner Gate (“Neiguan” point): Located three finger-widths above the wrist crease, between two tendons. Stimulating this point may ease discomfort in the heart, chest, and stomach.
- Spirit Gate (“Shenmen” point): Located at the inner wrist crease on the pinky side in a small hollow. Applying pressure here may promote relaxation and a calming effect.
- Peaceful Sleep (“Anmian” point): Located in the hollow between the mastoid bone (behind the ear) and the hairline. Gentle tapping here may help reduce stress and support better sleep, even without pinpoint accuracy.
4. Herbs
Some herbs may aid in breast cancer treatment and recovery:
- Green Tea: Rich in polyphenols, such as epigallocatechin-3-gallate, which may help slow tumor growth.
- Echinacea: Contains flavonoids that stimulate the immune system. Preclinical studies suggest it may inhibit the progression of breast cancer in laboratory models.
5. Music Therapy
Music therapy is a supportive tool in cancer care that may reduce treatment side effects such as pain, nausea, fatigue, anxiety, and depression. It promotes emotional well-being, boosts immune function, and enhances treatment adherence. Research shows that it can lower stress, reduce the need for medication, and improve both physical and emotional health.
6. Art Therapy
A 2019 study involving 20 women who had completed primary treatment for breast cancer explored the effects of art therapy compared to mandala coloring. Over eight weeks, participants in the art therapy group showed greater improvements in emotional awareness, acceptance of emotions, and reduced depressive symptoms. These benefits suggest that processing emotions through art therapy may help reduce both psychological and physical symptoms during cancer recovery.
[shortcut_anchor id=”anchor_1759527772178″ label=”Mindset”]How Does Mindset Affect Breast Cancer?[/shortcut_anchor]
Research shows that a positive, resilient mindset can greatly improve how people manage treatment and overall well-being. Support systems also play a key role in building this mindset.
A 2020 meta-analysis involving more than 282,000 breast cancer patients found that depression and anxiety significantly raised the risk of cancer recurrence and mortality. When both conditions were present, outcomes worsened even more.
Cultivating a resilient, positive outlook may be just as important as medical treatment in supporting recovery and improving long-term outcomes. A positive mindset has been linked to less pain, reduced psychological distress and depression, stronger feelings of support, better adherence to treatment plans, greater tolerance for side effects, and improved overall quality of life.
[shortcut_anchor id=”anchor_1759527777729″ label=”Prevention”]How Can I Prevent Breast Cancer?[/shortcut_anchor]
While breast cancer cannot always be prevented, certain steps may help lower risk. These measures may also reduce the risk of breast cancer recurrence.
1. Dietary Measures
A healthy diet supports breast health and overall well-being. Recommendations include:
- Follow a diet rich in whole, fresh foods, with plenty of fresh fruits, leafy greens, whole grains, and healthy fats.
- Eat foods that help eliminate excess estrogen from the body, such as leafy greens, cauliflower, and broccoli.
- Reduce intake of processed sugars, alcohol, and saturated fats.
- Ensure sufficient vitamin D levels.
- Limit alcohol use.
2. Lifestyle Habits
Daily lifestyle choices can also influence breast cancer risk. Helpful steps include:
- Engage in regular physical activity, including both weight-bearing and cardiovascular exercises.
- Maintain a healthy body weight.
- Get regular, high-quality sleep.
- Avoid exposure to endocrine-disrupting chemicals in plastics, pesticides, Bisphenol A, and polychlorinated biphenyls, two types of industrial chemicals.
- Breastfeed for several months after childbirth to help reduce breast cancer risk; breastfeeding also lowers recurrence risk in one subtype of breast cancer.
3. Certain Medications
Several drugs are approved to prevent breast cancer in women at higher risk. They can also reduce recurrence risk:
- Tamoxifen: For women 35 and older at high risk
- Raloxifene: For breast cancer prevention in postmenopausal women
For women who have never had breast cancer, regular screenings remain the best way for them to detect breast cancer early, when treatment is most effective.
4. Regular Breast Cancer Screenings
The U.S. Preventive Services Task Force recommends that all women ages 40 to 74 get screened for breast cancer every two years to reduce their risk of dying from the disease, with particular emphasis on ensuring black women begin screening at age 40.
For women at higher-than-average risk—such as those with genetic mutations or early chest radiation exposure—the American College of Radiology advises starting annual breast MRI screenings between ages 25 and 30, alongside annual mammograms that begin between ages 25 and 40, depending on individual risk factors. In some cases, mutation carriers may delay mammograms until age 40 if they undergo the recommended annual MRI screenings.
There is debate over whether screening should be done for everyone at an early age and at a high frequency.
[shortcut_anchor id=”anchor_1759527788050″ label=”Complications”]What Are the Possible Complications of Breast Cancer?[/shortcut_anchor]
Being diagnosed with breast cancer and undergoing treatment can result in various complications, such as:
- Increased Fatigue: Common and persistent, often caused by cancer, treatments, hormonal changes, stress, and emotions
- Emotional and Psychosocial Stress: Fluctuating emotions that place strain on daily life
- Lymphedema: Swelling from lymph fluid buildup after lymph tissue removal
- Menopausal Symptoms: Triggered by hormonal imbalances or treatments such as chemotherapy and hormone therapy
- Bone Health Issues: Reduced bone density from hormonal therapies, increasing fracture risk
- Cardiovascular Issues: Heart tissue damage or other side effects from radiation and certain chemotherapy drugs
When breast cancer goes undiagnosed or untreated, it can result in complications such as:
- Systemic Progression: Spread of cancer throughout the body, often to the bones, lungs, liver, or brain
- Reduced Quality of Life: Persistent pain and other lasting symptoms
- Metastatic Spread: Spread of cancer cells from the original tumor to other organs
- Death: The most serious outcome of untreated breast cancer