A study published in August suggests that hormonal contraceptives may influence how women process fear, with effects that could last even after stopping the medication.
Women using hormonal contraceptives showed significantly higher fear responses in safe environments compared with women who had never used birth control.
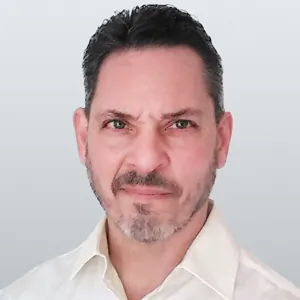
“It could explain why anxiety and fear-related disorders are more common in women,” Dr. Tiao-Virirak Kattygnarath, fertility expert and fellow of the American College of Obstetricians and Gynecologists, and not involved in the study, told The Epoch Times.
The research “directly demonstrates” that oral contraceptives influenced participants’ behavior, he added.
Electric Shocks Used to Elicit Fear
The study, published in Nature, involved 147 healthy participants, including men, women with natural menstrual cycles, and women using hormonal contraceptives. All women on contraceptives used only combined contraceptives.
Researchers designed a two-day experiment to test how well participants could distinguish between threatening and safe situations.
On the first day, participants learned to associate the turning off of certain colored lights with receiving an electric shock in an office environment (the threatening environment). They then learned that in a library (the safe environment), the lights in a lamp were turned off without their receiving shocks.
On the second day, researchers tested whether fear responses returned when lamps were turned off in both contexts by measuring skin reactions and brain activity.
Women who were currently using hormonal contraceptives or had used them in the past continued to exhibit fear responses when placed in the safe environments—essentially failing to recognize they were no longer in danger.
Specifically, those who had higher doses of synthetic estrogen in their contraceptives displayed greater fear return in safe settings. These effects persisted beyond discontinuing the contraceptives, suggesting that the hormone has a long-lasting influence on behavior.
Women with natural hormonal fluctuations did not show the same impaired safety responses.
“It’s significant that synthetic hormones in oral contraceptives appear to have a different impact than natural hormonal fluctuations,” Kattygnarath said. “This suggests the continuous, higher-dose exposure can change fear processing,” with important implications for mental health.
Brain scans revealed the biological mechanism behind the behavioral changes. Women using contraceptives showed decreased activity in the hippocampus and ventromedial prefrontal cortex, which are brain regions crucial for distinguishing between real threats and safe situations.
When brain activity is reduced, it becomes harder for women to suppress fear in safe contexts.
According to the study, the impairment could be caused by a direct effect of the synthetic hormones on brain circuits involved in learning and emotional memory. If given during adolescence, it could disrupt regulation systems that are still developing.
Broader Implications
The study highlights the importance of considering hormonal influences when understanding fear-related disorders such as PTSD, which can be two to three times more common in women.
Dr. Trisha Shah, a reproductive endocrinologist at Conceptions Florida, and not involved in the study, emphasized that clinicians can utilize the Centers for Disease Control and Prevention guidelines for U.S. Medical Eligibility Criteria for Contraceptive Use.
“In this evidence-based guideline, combined oral contraceptives were not associated with increased mental health symptoms in women with underlying depression or bipolar disorder,” she told The Epoch Times. “They are considered safe to prescribe in these cases, but more research is needed to understand better the potential adverse effects of contraceptives and mental health.”
In general, Shah continued, she screens patients regarding their mental health when counseling about hormonal contraceptives and discusses their possible mood-related effects and the potential benefits, which include menstrual cycle regulation, management of pain or bleeding, contraception, and management of acne.
“It should be a shared decision-making process between the physician and patient,” she said.
Study Limitations
Researchers noted the study had some limitations.
It was conducted on healthy individuals with brief exposure to different environments, which might not fully capture real-world fear responses. The sample was homogeneous and may not represent women with existing mental health conditions.
Further research is needed to confirm these findings in clinical populations and to explore how different contraceptive formulations and doses impact fear processing over time.
Understanding this influence could inform better contraceptive choices and mental health treatments tailored to women’s biological responses to fear.